Negative Symptoms of Schizophrenia: An Intervention-Focused Clinical Perspective
 Negative symptoms represent the core disabling dimension of schizophrenia. While positive symptoms bring patients to clinical attention, negative symptoms determine whether they return to education, employment, relationships, and independent living.
Negative symptoms represent the core disabling dimension of schizophrenia. While positive symptoms bring patients to clinical attention, negative symptoms determine whether they return to education, employment, relationships, and independent living.
Despite decades of research, negative symptoms remain undertreated—not because they are untreatable, but because they are often misidentified, oversimplified, or approached with blunt tools.
This article focuses on what can realistically be done, today, using pharmacological strategies and neuromodulation approaches such as rTMS and tDCS, within a personalised, neuroscience-informed framework.
Understanding the Target: What Are We Treating?
Negative symptoms are not a single entity. They cluster into two broad domains:
1. Experiential Deficits
-
Avolition (loss of motivation)
-
Anhedonia (reduced anticipation of pleasure)
-
Asociality
These are closely linked to reward processing and goal-directed behaviour, mediated by fronto-striatal circuits.
2. Expressive Deficits
-
Blunted affect
-
Alogia
These reflect impaired emotional expression and spontaneous communication, associated with prefrontal and limbic dysconnectivity.
This distinction matters because interventions do not affect all domains equally.
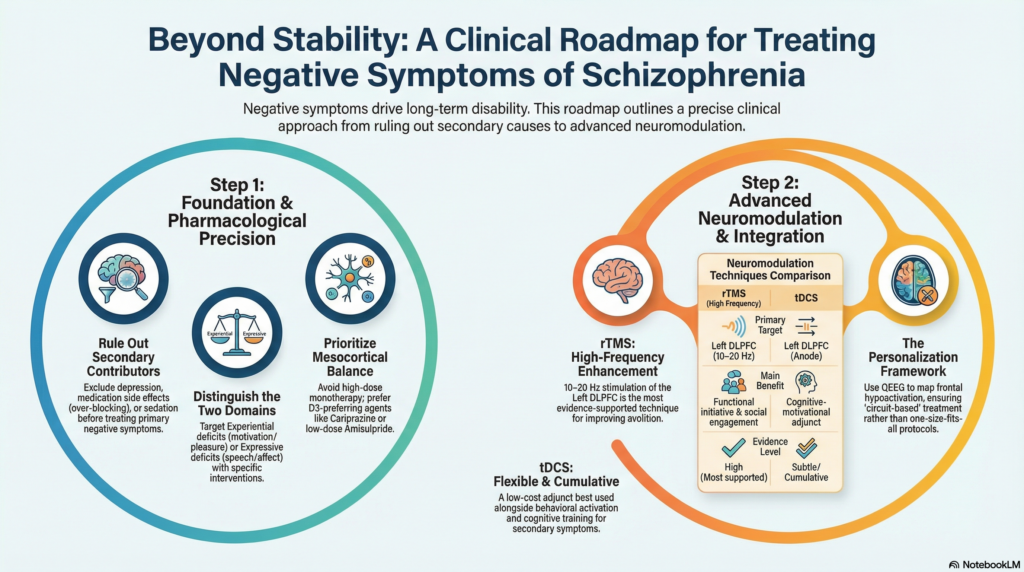
Step One: Rule Out Secondary Negative Symptoms
Before escalating treatment, clinicians must systematically exclude secondary contributors, which are often reversible:
-
Residual psychosis
-
Depression (including post-psychotic depression)
-
Extrapyramidal symptoms
-
Antipsychotic over-blocking
-
Sedation, social deprivation, institutionalisation
Failure to do this leads to the common error of “treating negative symptoms” while actually perpetuating them pharmacologically.
Pharmacological Interventions: Precision Over Potency
1. Optimising Antipsychotic Strategy
Negative symptoms worsen when dopamine blockade exceeds what is required for psychosis control.
Key principles:
-
Avoid high-dose antipsychotic monotherapy
-
Avoid irrational polypharmacy
-
Prefer agents with better mesocortical dopamine preservation
Relatively favourable profiles include:
-
Amisulpride (low–moderate dose range)
-
Cariprazine (D3-preferring partial agonism)
-
Aripiprazole (selective cases, careful monitoring)
Dose reduction alone—when clinically safe—can sometimes lead to marked improvement in motivation and expressivity.
2. Antidepressants: Targeting Secondary and Overlapping Domains
SSRIs and SNRIs do not treat primary negative symptoms, but they are invaluable when:
-
Depression masquerades as avolition
-
Anxiety contributes to withdrawal
-
Emotional blunting is misattributed to schizophrenia
Bupropion and vortioxetine are occasionally useful for activation and cognitive-motivational overlap, though evidence remains mixed.
3. Adjunctive Strategies (Selective Use)
-
Modafinil / armodafinil: limited but situational benefit
-
Memantine: modest effects in select profiles
-
Anti-inflammatory or glutamatergic agents: experimental, evolving
The overarching principle remains: less blockade, more balance.
rTMS for Negative Symptoms: Evidence-Based Neuromodulation
Repetitive Transcranial Magnetic Stimulation (rTMS) is currently the most evidence-supported neuromodulation technique for negative symptoms.
Why rTMS Works (When It Works)
Negative symptoms are associated with hypoactivity of the left dorsolateral prefrontal cortex (DLPFC). High-frequency rTMS increases cortical excitability and network efficiency in this region.
Typical Protocols
-
Target: Left DLPFC
-
Frequency: 10–20 Hz
-
Sessions: 20–30
-
Intensity: ~100–120% motor threshold
What Improves Most?
-
Avolition
-
Blunted affect
-
Social engagement
-
Functional initiative
Clinical Reality
-
Best results in early illness
-
Better outcomes when positive symptoms are stable
-
Less effective in severe primary deficit syndrome
rTMS should be seen as a functional enhancer, not a rescue intervention.
tDCS: A Low-Cost, High-Precision Adjunct
Transcranial Direct Current Stimulation (tDCS) is quieter, cheaper, and more flexible—but demands careful patient selection.
Mechanism
tDCS modulates neuronal membrane potentials, enhancing or inhibiting cortical excitability depending on polarity.
Common Negative Symptom Montage
-
Anode: Left DLPFC
-
Cathode: Right supraorbital / contralateral prefrontal region
-
Intensity: 1–2 mA
-
Duration: 20–30 minutes
-
Sessions: 10–20
Where tDCS Fits Best
-
Secondary negative symptoms
-
Cognitive-motivational deficits
-
Adjunct to pharmacological optimisation
-
Academic and research-guided clinical settings
Unlike rTMS, tDCS is subtle but cumulative. Its strength lies in integration with behavioural activation and cognitive training, not stand-alone use.
Role of QEEG and Personalisation
Not all negative symptoms arise from the same cortical dynamics.
QEEG can help identify:
-
Frontal hypoactivation
-
Inefficient state regulation
-
Network asymmetries
This allows:
-
Better selection of rTMS vs tDCS
-
Avoidance of “protocol-driven” neuromodulation
-
Objective pre–post functional assessment
Ruthless standardisation harms neuromodulation’s reputation. Personalisation restores it.
Integrating Interventions: A Practical Framework
-
Stabilise positive symptoms
-
Identify and treat secondary contributors
-
Optimise antipsychotic dosing and choice
-
Add neuromodulation (rTMS or tDCS) when indicated
-
Pair with structured behavioural activation
-
Measure functional outcomes—not just symptom scales
Recovery emerges from alignment, not escalation.
Looking Forward: From Symptom Control to Functional Restoration
Negative symptoms are not an afterthought of schizophrenia—they are its functional core.
Modern psychiatry must move beyond:
-
“Symptoms controlled”
-
“Patient stable”
Toward:
-
Motivation restored
-
Agency regained
-
Life re-entered
Pharmacology sets the foundation. Neuromodulation reshapes circuits. Purpose completes recovery.
Dr. Srinivas Rajkumar T, MD (AIIMS, New Delhi), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery
📞 +91-8595155808