Models of Executive Functioning in ADHD
Attention-Deficit/Hyperactivity Disorder (ADHD) is often reduced to problems of attention or impulsivity. Clinically, however, what most adults and adolescents struggle with is something broader and more disabling: executive dysfunction—difficulty organizing behavior over time in the service of goals.
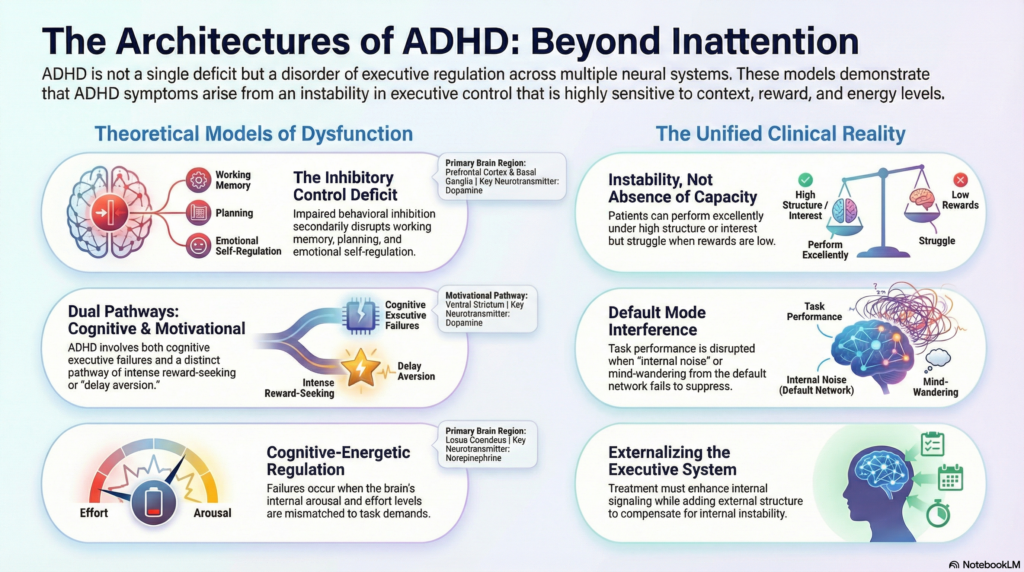 Over the past three decades, several theoretical models have attempted to explain why executive control fails in ADHD. Each model captures a different layer of the disorder, and together they reveal an important truth: ADHD is not a single executive deficit, but a disorder of executive regulation across multiple systems.
Over the past three decades, several theoretical models have attempted to explain why executive control fails in ADHD. Each model captures a different layer of the disorder, and together they reveal an important truth: ADHD is not a single executive deficit, but a disorder of executive regulation across multiple systems.
1. Barkley’s Inhibitory Control Model
ADHD as a disorder of behavioral inhibition
Russell Barkley’s model is one of the most influential and clinically intuitive frameworks.
Core idea
The primary deficit in ADHD is impaired behavioral inhibition, which secondarily disrupts other executive functions.
According to Barkley, inhibition failure leads to impairment in:
-
Working memory (especially non-verbal)
-
Internalization of speech
-
Self-regulation of affect and motivation
-
Reconstitution (planning and problem-solving)
Neurobiological grounding
-
Frontostriatal circuitry (PFC–basal ganglia)
-
Dopaminergic modulation of inhibitory control
-
Delayed maturation of prefrontal cortex
Clinical strength
Explains:
-
Impulsivity
-
Emotional dysregulation
-
“Knowing what to do but not doing it”
Limitation
Does not fully explain:
-
Pure inattentive presentations
-
Motivational variability
-
Delay aversion
2. Dual Pathway Model
ADHD as executive dysfunction and motivational dysregulation
Proposed by Sonuga-Barke, this model challenged the idea that ADHD is purely an executive disorder.
Core idea
There are two partially independent pathways to ADHD symptoms:
-
Executive dysfunction pathway
-
Deficits in inhibition, working memory, planning
-
-
Motivational pathway (delay aversion)
-
Strong preference for immediate rewards
-
Difficulty tolerating delay
-
Neurobiological grounding
-
Executive pathway: frontoparietal control network
-
Motivational pathway: ventral striatum, orbitofrontal cortex
Clinical strength
Explains:
-
Why some patients perform well under urgency
-
Why rewards dramatically change behavior
-
Variability across contexts
Limitation
Still treats executive functions as relatively unitary within the cognitive pathway.
3. Cognitive–Energetic Model
ADHD as impaired regulation of mental effort
Proposed by Sergeant, this model reframes executive dysfunction as a problem of state regulation, not capacity.
Core idea
ADHD reflects difficulty regulating:
-
Arousal
-
Activation
-
Effort
Executive failures occur when energetic state is mismatched to task demands.
Neurobiological grounding
-
Locus coeruleus–noradrenergic system
-
Dopamine–norepinephrine balance
-
Arousal networks interacting with PFC
Clinical strength
Explains:
-
Fluctuating performance
-
Fatigue with low-stimulation tasks
-
Improvement with novelty or challenge
Limitation
Less precise in mapping specific executive processes like planning or inhibition.
4. Executive Attention Network Model
ADHD as impaired top-down attentional control
This model emphasizes dysfunction in the executive attention system, particularly the ability to resolve conflict and maintain task goals.
Core idea
ADHD reflects weakness in the anterior cingulate–prefrontal network responsible for executive attention.
Neurobiological grounding
-
Anterior cingulate cortex (ACC)
-
Dorsolateral prefrontal cortex
-
Frontoparietal connectivity
Clinical strength
Explains:
-
Distractibility
-
Errors under cognitive load
-
Poor conflict monitoring
Limitation
Does not fully address emotional or motivational dysregulation.
5. Default Mode Interference Model
ADHD as failure to suppress internal noise
A more recent network-based perspective.
Core idea
In ADHD, the default mode network (DMN) intrudes during task performance due to inadequate suppression by executive networks.
Neurobiological grounding
-
Reduced anticorrelation between DMN and task-positive networks
-
Network-level dysregulation rather than focal deficits
Clinical strength
Explains:
-
Mind-wandering
-
“Zoning out”
-
Task-unrelated thoughts
Limitation
Descriptive rather than mechanistic at the behavioral level.
6. Network Dysregulation Model (Contemporary View)
ADHD as large-scale network imbalance
Modern neuroimaging suggests ADHD is best understood as a disorder of network coordination, not isolated executive modules.
Key networks involved:
-
Frontoparietal control network
-
Salience network
-
Default mode network
-
Reward and motivational circuits
Core idea
ADHD reflects unstable switching and poor synchronization between networks required for sustained, goal-directed behavior.
This model integrates:
-
Executive deficits
-
Motivational variability
-
Emotional dysregulation
-
Context dependence
A unifying clinical insight
Across models, one theme recurs:
ADHD is not an absence of executive capacity, but an instability in executive control.
Patients can demonstrate:
-
Excellent performance under the right conditions
-
Severe impairment under low structure or low reward
This explains why ADHD often goes unrecognized in intelligent, high-functioning individuals—and why structure, interest, and immediacy can temporarily “normalize” functioning.
Implications for assessment and treatment
Understanding these models guides practice:
-
Assessment should go beyond attention tests to include:
-
Working memory
-
Inhibition
-
Delay tolerance
-
Emotional regulation
-
-
Treatment works best when it:
-
Enhances executive signaling (stimulants)
-
Modulates arousal and motivation
-
Adds external structure to compensate for internal instability
-
Trains executive endurance, not just speed
-
Closing reflection
ADHD is often misunderstood because it looks inconsistent. But inconsistency is the diagnosis.
Executive functioning in ADHD is not broken—it is context-sensitive, energy-dependent, and reward-responsive. The various models do not contradict each other; they describe different cross-sections of the same neurobiological reality.
Understanding these models allows clinicians to move from labeling deficits to designing environments where executive function can actually emerge.
Dr. Srinivas Rajkumar T, MD (AIIMS, New Delhi), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall)
✉ srinivasaiims@gmail.com 📞 +91-8595155808