EO-OCD (Early-Onset Obsessive-Compulsive Disorder): Challenges in Diagnosis and Treatment
 Early-Onset Obsessive-Compulsive Disorder (EO-OCD) refers to OCD that begins in childhood or early adolescence, typically before 12–13 years of age. Far from being a milder or temporary version of adult OCD, EO-OCD is now understood as a distinct neurodevelopmental subtype, with unique clinical patterns, biological underpinnings, and long-term implications.
Early-Onset Obsessive-Compulsive Disorder (EO-OCD) refers to OCD that begins in childhood or early adolescence, typically before 12–13 years of age. Far from being a milder or temporary version of adult OCD, EO-OCD is now understood as a distinct neurodevelopmental subtype, with unique clinical patterns, biological underpinnings, and long-term implications.
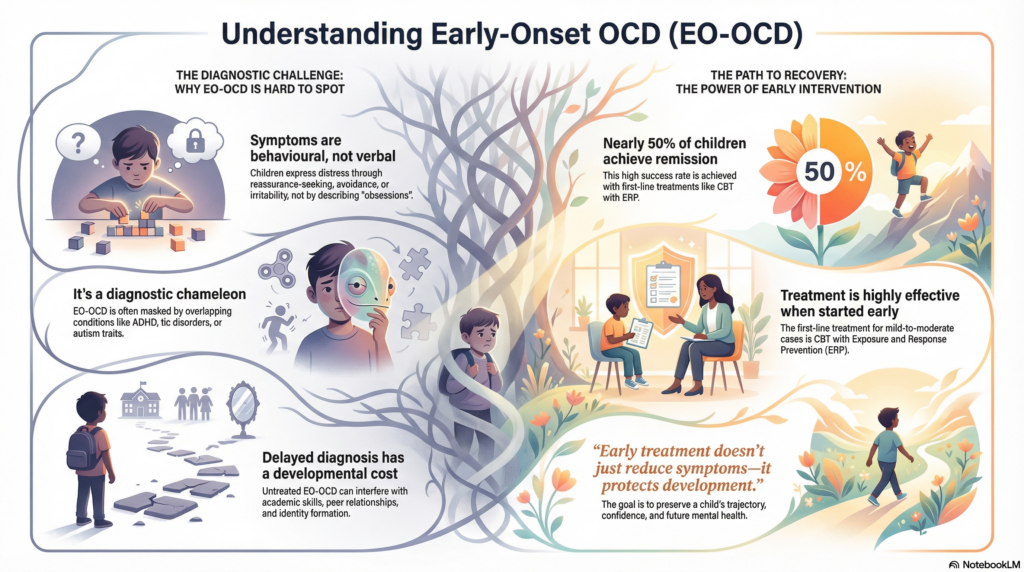
Recognising EO-OCD early can be life-altering. Missing it can quietly reshape a child’s emotional, cognitive, and social development.
What Makes EO-OCD Different?
EO-OCD differs from adult-onset OCD in several important ways:
-
Earlier brain circuit involvement, especially cortico-striato-thalamo-cortical (CSTC) loops during critical developmental windows
-
Higher rates of comorbidity, particularly ADHD, tic disorders, and neurodevelopmental traits
-
Reduced insight, with children often believing their obsessions are realistic, necessary, or morally correct
-
Greater family involvement, both as buffers and, unintentionally, as maintainers of symptoms
These differences explain why EO-OCD is frequently misdiagnosed, underdiagnosed, or diagnosed late.
Diagnostic Challenges in EO-OCD
1. Limited Insight and Language
Children rarely describe “obsessions” clearly. Instead, they present with:
-
Excessive reassurance-seeking
-
Avoidance of everyday situations
-
Irritability or emotional outbursts when rituals are blocked
-
Somatic complaints or school refusal
Because insight develops later, distress may be expressed behaviourally rather than verbally.
2. The Subclinical Overlap
Around 10–15% of children show subclinical obsessive-compulsive symptoms. Developmentally normal rituals (bedtime routines, counting games, superstitions) can mask early pathology, leading to a prolonged duration of untreated illness (DUI).
3. Comorbidity as Camouflage
EO-OCD is a diagnostic chameleon:
-
ADHD: Intrusive thoughts disrupt attention, mimicking inattentive ADHD
-
Tic disorders: A well-recognised overlap exists, sometimes labelled Obsessive-Compulsive Tic Disorder (OCTD)
-
Autism spectrum traits: Rigidity and repetitive behaviours blur boundaries and require adapted assessment strategies
If OCD is not actively looked for, it is easily missed.
4. Developmental Cost of Delay
Delayed diagnosis is not neutral. EO-OCD can interfere with:
-
Academic skill acquisition
-
Peer relationships
-
Emotional regulation
-
Identity formation
Over time, maladaptive coping patterns can become entrenched well into adulthood.
Treatment Challenges in EO-OCD
Evidence-Based Care Still Works Best
Despite its complexity, EO-OCD responds well to structured treatment when started early:
-
CBT with Exposure and Response Prevention (ERP) is first-line for mild to moderate EO-OCD
-
CBT + SSRIs is recommended for moderate to severe cases
Children’s brains are more plastic, making early intervention particularly powerful.
Biological Complexity Beyond Serotonin
EO-OCD is not just a serotonin disorder:
-
Glutamatergic dysregulation has been strongly implicated, prompting interest in adjuncts such as N-acetylcysteine (NAC) and memantine in resistant cases
-
Immune-mediated subtypes, including PANS/PANDAS, may present with abrupt onset and benefit from immunomodulatory strategies
-
Neuroinflammation and microglial activation are emerging areas of interest
-
Gut–brain axis influences overlap with sensitive periods of neurodevelopment, opening future avenues for adjunctive care
This reflects a broader move toward precision psychiatry in pediatric OCD.
Why Early Intervention Matters More in EO-OCD
One of the most hopeful findings in child psychiatry is that EO-OCD has better remission rates than adult-onset OCD. Nearly half of children achieve remission with first-line treatments.
Factors associated with better outcomes include:
-
Early identification and treatment
-
Treating OCD before targeting secondary attentional symptoms
-
Reducing family accommodation
-
Active parental involvement in therapy
Early treatment doesn’t just reduce symptoms—it protects development.
Key Takeaway
EO-OCD is a neurodevelopmental, multisystem disorder, not a behavioural problem or personality trait. Its challenges lie in subtle presentation, overlapping diagnoses, and biological heterogeneity—but its greatest strength is treatability when recognised early.
The goal in EO-OCD is not merely symptom control. It is preserving a child’s developmental trajectory, confidence, and future mental health.
Dr. Srinivas Rajkumar T, MD (AIIMS, New Delhi)
Consultant Psychiatrist
Apollo Clinic Velachery (Opp. Phoenix Mall)
✉ srinivasaiims@gmail.com 📞 +91-8595155808