Role of qEEG in Obsessive–Compulsive Disorder (OCD)
 Obsessive–Compulsive Disorder (OCD) is often misunderstood as a problem of excessive anxiety or weak self-control. In reality, OCD is a disorder of persistence—of thoughts that refuse to stop, doubts that refuse to settle, and mental loops that refuse to disengage, even when the person clearly recognises their irrational nature.
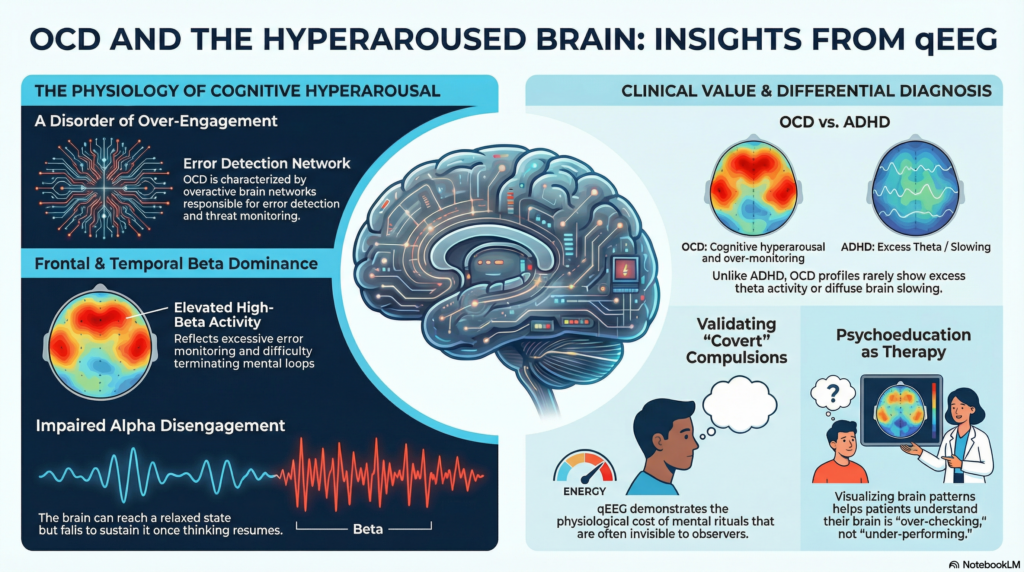
Obsessive–Compulsive Disorder (OCD) is often misunderstood as a problem of excessive anxiety or weak self-control. In reality, OCD is a disorder of persistence—of thoughts that refuse to stop, doubts that refuse to settle, and mental loops that refuse to disengage, even when the person clearly recognises their irrational nature.
In recent years, quantitative EEG (qEEG) has attracted attention in the assessment and treatment of OCD. Some portray it as a diagnostic breakthrough, while others dismiss it entirely. The truth lies in between. qEEG does not diagnose OCD, but when used thoughtfully, it helps us understand why obsessions persist and why certain treatments work.
OCD is not a disorder of weak thinking
A common myth about OCD is that affected individuals have poor attention or weak memory. Clinically, the opposite is often true. Many people with OCD are intelligent, detail-oriented, and highly self-aware. Their difficulty lies not in generating thoughts, but in stopping them.
OCD involves overactivation of brain networks responsible for:
-
Error detection
-
Threat monitoring
-
Cognitive control
The brain behaves like an overzealous quality-control system—never satisfied, never signing off.
This is where qEEG becomes useful.
What qEEG actually measures
qEEG is a quantitative analysis of the brain’s electrical activity recorded using EEG. It evaluates:
-
Brain wave frequencies (delta, theta, alpha, beta)
-
Their distribution across brain regions
-
How these patterns change between rest and task states
qEEG does not show thoughts, emotions, or memories directly. Instead, it reflects the functional state of cortical activation—whether the brain is under-aroused, balanced, or over-driven.
Typical qEEG patterns seen in OCD
Across clinical experience and research literature, OCD commonly shows a pattern of cognitive hyperarousal rather than cognitive deficit.
Frontal and temporal beta dominance
Many individuals with OCD show elevated beta and high-beta activity in frontal and anterior temporal regions.
This pattern reflects:
-
Excessive error monitoring
-
Persistent internal speech
-
Overactive cognitive control
-
Difficulty terminating mental loops
It is especially prominent in patients with:
-
Obsessional doubt
-
Mental checking
-
Rumination
-
“Pure obsessional” OCD
This is not chaotic anxiety. It is precision anxiety—the brain demanding certainty before letting go.
Preserved alpha rhythm with poor disengagement
In OCD, alpha rhythm is often:
-
Normal at rest
-
Reactive during eye closure
-
Poorly sustained once thinking resumes
In simple terms:
The brain can relax, but it does not stay relaxed.
This mirrors the lived experience of OCD—temporary reassurance followed by rapid return of doubt and the urge to “just check once more.”
What is not seen is equally important
Most OCD qEEG profiles do not show:
-
Excess theta activity
-
Diffuse slowing
-
Disorganised rhythms
This helps distinguish OCD from ADHD, organic brain dysfunction, or neurocognitive disorders. OCD is not a disorder of low brain power—it is a disorder of over-engagement.
Why qEEG does not diagnose OCD
qEEG should never replace clinical assessment. It:
-
Does not confirm or exclude OCD on its own
-
Does not replace detailed clinical interviews
-
Cannot reliably subtype OCD
Without clinical context, qEEG data can mislead. Used responsibly, it complements—not competes with—good psychiatry.
Where qEEG adds real value in OCD
Differential diagnosis
qEEG can help differentiate OCD from:
-
ADHD
-
Depressive rumination
-
Psychotic disorders presenting with intrusive thoughts
This is particularly useful in complex or overlapping presentations.
Understanding covert compulsions
Many people with OCD perform compulsions entirely in the mind—silent repetition, mental checking, or internal reassurance. These are often missed by questionnaires.
qEEG helps demonstrate the physiological cost of mental compulsions, validating the patient’s experience even when screening scales appear “normal.”
Guiding adjunctive interventions
In specialised settings, qEEG can assist in:
-
Planning neurofeedback protocols
-
Monitoring physiological change over time
-
Supporting neuromodulation strategies
These approaches remain adjunctive to standard care.
Psychoeducation and engagement
For many patients, especially high-functioning individuals, understanding that their brain is over-checking rather than under-performing reduces shame and improves engagement with therapy, particularly Exposure and Response Prevention (ERP).
qEEG and treatment: knowing its place
The cornerstone treatments for OCD remain:
-
SSRIs
-
Cognitive Behaviour Therapy with ERP
qEEG does not choose medications or replace therapy. Its role is to explain resistance, guide adjuncts, and support persistence with evidence-based care.
ERP works because it retrains the brain to disengage without certainty—exactly what qEEG suggests is failing in OCD.
In OCD, qEEG is not a diagnostic test but a lens—revealing cognitive hypervigilance and impaired disengagement, helping clinicians refine diagnosis, guide adjunctive care, and help patients understand their minds with clarity and compassion.
About the Author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Dr. Srinivas Rajkumar practices evidence-based psychiatry with a strong focus on OCD, anxiety disorders, adult ADHD, and neuropsychiatric conditions. His work integrates careful clinical formulation with tools such as qEEG, neurofeedback, and cognitive neuroscience-informed psychotherapy, while maintaining strict adherence to ethical and scientific standards.
He currently consults at Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall), Chennai, and is actively involved in teaching, research, and public mental health education.
✉ srinivasaiims@gmail.com
📞 +91-8595155808