QEEG-Guided tDCS in Depression, Anxiety, and OCD: Moving From Labels to Brain-Based Care
 Modern psychiatry is quietly undergoing a shift.
Modern psychiatry is quietly undergoing a shift.
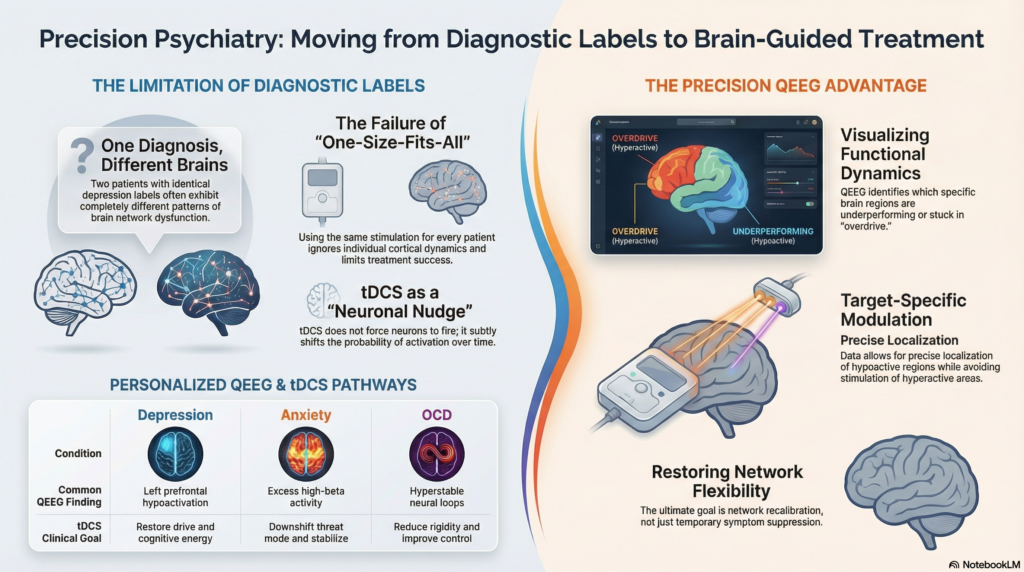
For decades, we have treated depression, anxiety, and obsessive–compulsive disorder largely through diagnostic labels and symptom clusters. While this approach has helped millions, it has also revealed its limits. Two patients with the same diagnosis often respond very differently to the same treatment. Some improve dramatically. Others plateau. A few worsen.
This inconsistency has forced an uncomfortable but necessary question:
Are we treating disorders—or are we treating brains?
Quantitative EEG (QEEG)–guided transcranial direct current stimulation (tDCS) represents one of the most practical steps toward answering that question in day-to-day clinical practice.
Why Diagnosis Alone Is Not Enough
Depression, anxiety, and OCD are not single diseases. They are final common pathways—clinical syndromes emerging from different patterns of brain network dysfunction.
A patient with depression may present with:
-
Psychomotor slowing and apathy
-
Or agitation and intrusive rumination
An anxious patient may show:
-
Fear-driven hyperarousal
-
Or cognitive overcontrol with emotional suppression
An OCD patient may be dominated by:
-
Motoric compulsions
-
Or purely cognitive obsessions
Treating all of these with the same neuromodulation montage simply because the DSM label is identical is conceptually flawed.
QEEG helps us step out of that trap.
What QEEG Really Offers (Beyond “Brain Mapping”)
QEEG is often misunderstood as a diagnostic tool. In reality, its greatest value lies elsewhere.
QEEG allows clinicians to visualise functional brain dynamics, including:
-
Regional over- or under-activation
-
Imbalances between hemispheres
-
Excessive slow or fast frequency activity
-
Poor network coordination
-
State regulation inefficiencies
In simple terms, QEEG answers:
-
Which regions are underperforming?
-
Which regions are stuck in overdrive?
-
Where is flexibility lost?
These answers are precisely what tDCS needs to be effective.
tDCS: Subtle, Cumulative, and Often Misused
tDCS is frequently marketed as “simple stimulation.” This description does it a disservice.
tDCS does not force neurons to fire. Instead, it nudges neuronal systems toward or away from activation, altering the probability of firing over repeated sessions. Over time, this shapes plasticity and network efficiency.
This makes tDCS:
-
Less dramatic than rTMS
-
Less immediately noticeable
-
But deeply dependent on accurate targeting and polarity selection
Without guidance, tDCS risks becoming placebo-adjacent. With guidance, it becomes a precision adjunct.
QEEG-Guided tDCS in Depression: Restoring Drive, Not Just Mood
The Neurobiology Behind the Symptoms
Many depressive syndromes are characterised not just by sadness, but by:
-
Loss of initiative
-
Cognitive fatigue
-
Rumination
-
Emotional blunting
QEEG frequently reveals:
-
Left prefrontal hypoactivation
-
Frontal alpha asymmetry
-
Excess theta activity in executive regions
-
Reduced frontal network efficiency
These patterns reflect reduced top-down control over mood and cognition.
How QEEG Shapes tDCS Decisions
Instead of a fixed “left DLPFC anode for all,” QEEG allows:
-
Precise localisation of hypoactive frontal regions
-
Avoidance of stimulating already hyperactive areas
-
Tailoring polarity to individual cortical dynamics
Clinically, this translates into:
-
Improved psychomotor energy
-
Reduced rumination
-
Better antidepressant responsiveness
-
Greater engagement with psychotherapy
tDCS does not replace medication in depression. It amplifies what medication struggles to restore: motivation and cognitive energy.
QEEG-Guided tDCS in Anxiety Disorders: Teaching the Brain to Stand Down
Anxiety Is Not Just “Too Much Fear”
Anxiety disorders often reflect failure of inhibition, not just excessive emotion.
Common QEEG findings include:
-
Excess high-beta activity
-
Right frontal dominance
-
Poor alpha stability
-
Inability to downshift from threat mode
These brains are not weak—they are overcommitted to vigilance.
The Role of tDCS in Anxiety
In anxiety, indiscriminate prefrontal excitation can worsen symptoms. QEEG helps prevent this.
tDCS strategies may involve:
-
Cathodal inhibition of hyperactive regions
-
Bilateral prefrontal balancing
-
Stabilisation rather than excitation
When used thoughtfully, tDCS can:
-
Reduce baseline arousal
-
Improve emotional regulation
-
Enhance tolerance for exposure-based therapies
-
Reduce dependence on sedative medications
In anxiety, tDCS works best as a neurophysiological primer—creating a calmer internal terrain for therapy to work.
QEEG-Guided tDCS in OCD: Softening Rigidity, Not Suppressing Thoughts
OCD is not merely about intrusive thoughts. It is about rigidity of neural loops.
QEEG often shows:
-
Excess beta activity in frontal or medial regions
-
Hyperstable networks
-
Poor cognitive flexibility
-
Overactive control circuits
These patterns align with the lived experience of OCD: knowing something is irrational, yet being unable to disengage.
Where tDCS Fits in OCD
tDCS does not “switch off” obsessions. Instead, it aims to:
-
Reduce circuit rigidity
-
Improve inhibitory control
-
Enhance responsiveness to ERP and CBT
QEEG helps decide:
-
Whether inhibition or facilitation is required
-
Whether medial frontal or lateral prefrontal regions are dominant drivers
-
How to titrate sessions safely to avoid symptom flare-ups
In OCD, tDCS is most useful in partial responders, where medication and therapy have helped—but not enough.
Why Non-Guided tDCS Often Disappoints
The growing skepticism around tDCS usually stems from how it is used, not from what it can do.
Common pitfalls include:
-
One-size-fits-all montages
-
Ignoring cortical hyperactivation
-
No baseline functional assessment
-
No integration with ongoing treatment
-
Treating tDCS as a shortcut
Neuromodulation without formulation is electrical guesswork.
Integrating QEEG-Guided tDCS Into Ethical Practice
A responsible clinical pathway looks like this:
-
Careful diagnostic and functional formulation
-
Baseline QEEG assessment
-
Identification of dominant network dysfunction
-
Individualised tDCS targeting and polarity
-
Integration with pharmacotherapy
-
Parallel psychotherapy or behavioural activation
-
Ongoing clinical monitoring
The goal is not symptom suppression, but network recalibration.
The Larger Shift: From Disorder-Centric to Brain-Centric Psychiatry
QEEG-guided tDCS does not represent futuristic psychiatry. It represents more careful psychiatry.
It acknowledges that:
-
Brains differ even when diagnoses match
-
Over-standardisation harms outcomes
-
Precision matters more than intensity
-
Technology must serve formulation, not replace it
tDCS is quiet.
Its effects are gradual.
Its success depends on humility and understanding.
When used well, it does not promise miracles—but it restores movement where the brain has become stuck.
Dr. Srinivas Rajkumar T, MD (AIIMS, New Delhi), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery
📞 +91-8595155808