Paroxetine FAQ
 Paroxetine is one of the earliest SSRIs introduced into clinical practice and has been used worldwide since the early 1990s. Over the years, it has helped millions of people with anxiety and depressive disorders, particularly those with severe anxiety, panic symptoms, and trauma-related conditions.
Paroxetine is one of the earliest SSRIs introduced into clinical practice and has been used worldwide since the early 1990s. Over the years, it has helped millions of people with anxiety and depressive disorders, particularly those with severe anxiety, panic symptoms, and trauma-related conditions.
Paroxetine has a distinct clinical profile. It is generally more calming and sedating than many other SSRIs and has a shorter half-life, which influences how it feels during treatment and how it needs to be stopped. Because of this, paroxetine is often misunderstood—sometimes described online as “strong” or “difficult,” without adequate explanation.
In India, paroxetine is widely available under brand names such as Paxil (original), Paxidep, Pari, Xet, and others. While brand names differ, the active medicine is the same, and treatment outcomes depend far more on appropriate dosing, careful monitoring, and individual suitability than on the brand itself.
This long clinical experience allows psychiatrists to use paroxetine selectively and thoughtfully—when its profile matches the patient’s needs.
Introduction
Being prescribed paroxetine often raises specific concerns.
Many patients ask:
Will this make me too sleepy? Will it cause weight gain? Is it hard to stop? Why was this chosen instead of another SSRI?
These are reasonable questions.
Paroxetine is not the right medication for everyone—but for some people, it can be particularly effective, especially when anxiety is intense, panic attacks are frequent, or emotional arousal is persistently high.
This article is written to explain paroxetine clearly—without exaggeration and without fear. The aim is not to promote or discourage its use, but to help you understand what it does, what it does not do, what is common, what is rare, and how it is usually used carefully in real clinical practice.
What does paroxetine do?
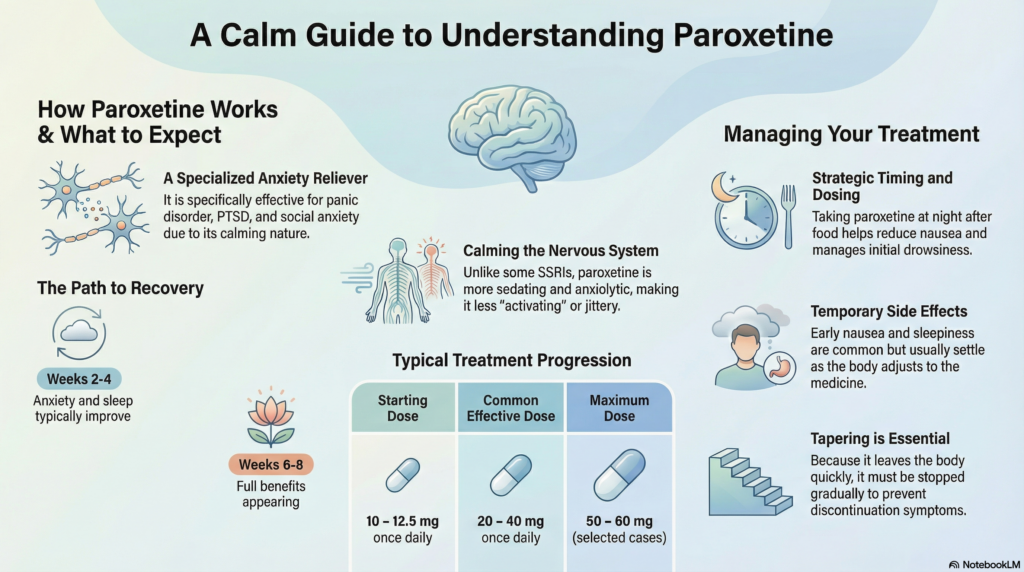
Paroxetine belongs to the group of medicines called SSRIs (Selective Serotonin Reuptake Inhibitors).
In simple terms, it:
-
Increases the availability of serotonin, helping regulate mood and anxiety
-
Reduces excessive fear responses and emotional hyperarousal
-
Has a calming effect on the nervous system
Compared to some other SSRIs, paroxetine is:
-
More sedating
-
More anxiolytic
-
Less activating
This makes it particularly useful in certain anxiety-dominant conditions.
Paroxetine is commonly prescribed for:
-
Panic disorder
-
Generalised anxiety disorder
-
Social anxiety disorder
-
Post-traumatic stress disorder (PTSD)
-
Depression with prominent anxiety or insomnia
What is the usual dose range of paroxetine?
Dosing is individualised and usually started low.
Typical ranges:
-
Starting dose: 10–12.5 mg once daily
-
Common effective dose: 20–40 mg once daily
-
Maximum dose: 50–60 mg (selected cases)
Slow dose increases are especially important with paroxetine to reduce side effects and improve tolerability.
Should paroxetine be taken with food or after food?
Paroxetine can be taken with or without food, but:
-
Taking it after food often reduces nausea
-
Food does not reduce its effectiveness
-
Taking it at the same time each day improves tolerability
Because of its sedating nature, paroxetine is often taken at night.
Does paroxetine make you sleepy or drowsy?
Yes, it can—especially early in treatment.
-
Many people feel sleepier or more relaxed initially
-
This effect often settles over time
-
For people with insomnia or severe anxiety, this can be helpful
If excessive drowsiness occurs:
-
Dose adjustment
-
Slower titration
-
Timing changes
can usually resolve it.
How long does paroxetine take to work?
Paroxetine works gradually, like other SSRIs.
-
Week 1–2: Side effects or mild calming effects may appear
-
Week 2–4: Anxiety, panic, and sleep often improve
-
Week 4–6: Mood, confidence, and emotional stability improve
-
Week 6–8: Full therapeutic benefit becomes clearer
Early side effects do not predict long-term response.
Does paroxetine make you emotionally numb?
This concern is understandable.
Most people experience:
-
Reduced emotional intensity
-
Better control over anxiety and fear
-
Improved emotional stability
A small minority, particularly at higher doses, may experience:
-
Emotional blunting
-
Reduced emotional range
Important points:
-
This effect is dose-related
-
It is reversible
-
Dose reduction or switching medication usually resolves it
The goal is calm clarity—not emotional suppression.
What are the common side effects?
Paroxetine tends to have more noticeable early side effects than some other SSRIs, but these are usually manageable.
Common:
-
Nausea
-
Sleepiness
-
Dry mouth
-
Constipation
-
Increased appetite or weight gain (in some people)
-
Sexual side effects
Less common:
-
Sweating
-
Headache
-
Mild dizziness
Most side effects improve with time, dose adjustment, or supportive strategies.
Does paroxetine cause dependence or addiction?
No.
Paroxetine does not:
-
Cause cravings
-
Produce a “high”
-
Lead to drug-seeking behaviour
However, because paroxetine has a short half-life, stopping it suddenly can cause discontinuation symptoms. This is not addiction—it reflects how quickly the drug leaves the body.
Will I have withdrawal symptoms if I stop paroxetine abruptly?
Paroxetine is more likely than other SSRIs to cause discontinuation symptoms if stopped suddenly.
Possible symptoms include:
-
Dizziness
-
Electric-shock sensations
-
Anxiety or irritability
-
Sleep disturbance
-
Flu-like feelings
To prevent this:
-
Paroxetine should be tapered slowly
-
Taper schedules are individualised
-
Most people stop comfortably with proper guidance
With correct tapering, discontinuation is usually smooth.
What is the risk of PSSD (Post-SSRI Sexual Dysfunction)?
PSSD refers to persistent sexual symptoms after stopping SSRIs.
Key points:
-
PSSD appears to be rare
-
Sexual side effects during treatment are more common than persistent symptoms
-
The majority of patients recover fully
-
Risk may be higher with long-term high-dose use, but remains uncommon
Sexual function is influenced by many factors:
-
Anxiety and depression themselves
-
Stress and fatigue
-
Sleep quality
-
Hormonal factors
-
Relationship issues
Early discussion allows timely management.
Are there alternatives to paroxetine?
Yes.
Alternatives may include:
-
Other SSRIs (e.g., sertraline, escitalopram)
-
SNRIs
-
Atypical antidepressants
-
Psychological therapies
-
Sleep-focused or trauma-focused interventions
Medication choice depends on symptom profile, side-effect sensitivity, and individual preference.
Is paroxetine safe during pregnancy or breastfeeding?
This requires a careful, individualised discussion.
-
Paroxetine is used less commonly than some other SSRIs during pregnancy
-
Risks and benefits must be weighed carefully
-
Untreated anxiety or depression also carries risks
Never stop medication suddenly during pregnancy without medical advice.
How long will I need to take paroxetine?
This varies:
-
First episode: usually 6–12 months after recovery
-
Panic disorder, PTSD, or recurrent anxiety: sometimes longer
Stopping medication is always a planned, gradual process.
Final thoughts
Paroxetine is not a “bad drug.”
It is a specific drug with a specific profile.
When used thoughtfully:
-
Anxiety and panic can reduce significantly
-
Sleep and emotional stability often improve
-
Quality of life can improve meaningfully
Good psychiatric care is about matching the right medication to the right nervous system, not about avoiding medications altogether.
Understanding reduces fear—and fear reduction itself is therapeutic.
About the author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic – Apollo Clinic Velachery (Opp. Phoenix Mall)
I provide evidence-based psychiatric care integrating medication, psychotherapy, sleep science, and modern neuropsychiatry—tailored to each individual.
✉ srinivasaiims@gmail.com
📞 +91-8595155808