Managing PMS and PMDD Without Medicines: Exercise, Neurofeedback, and Other Evidence-Based Strategies
 Not every woman with Premenstrual Syndrome (PMS) or Premenstrual Dysphoric Disorder (PMDD) wants medication. Some cannot tolerate it. Some prefer to avoid it. Others find that medicines help—but not enough on their own.
Not every woman with Premenstrual Syndrome (PMS) or Premenstrual Dysphoric Disorder (PMDD) wants medication. Some cannot tolerate it. Some prefer to avoid it. Others find that medicines help—but not enough on their own.
The good news is this:
PMS and PMDD are highly modifiable conditions, even without drugs, when management targets the brain–body systems that drive cyclical vulnerability.
This article looks at non-pharmacological approaches that actually make a difference—especially exercise, neurofeedback, sleep regulation, and psychological strategies.
First, a reality check
PMS and PMDD are not:
-
A lack of willpower
-
“Just stress”
-
A hormone imbalance in most cases
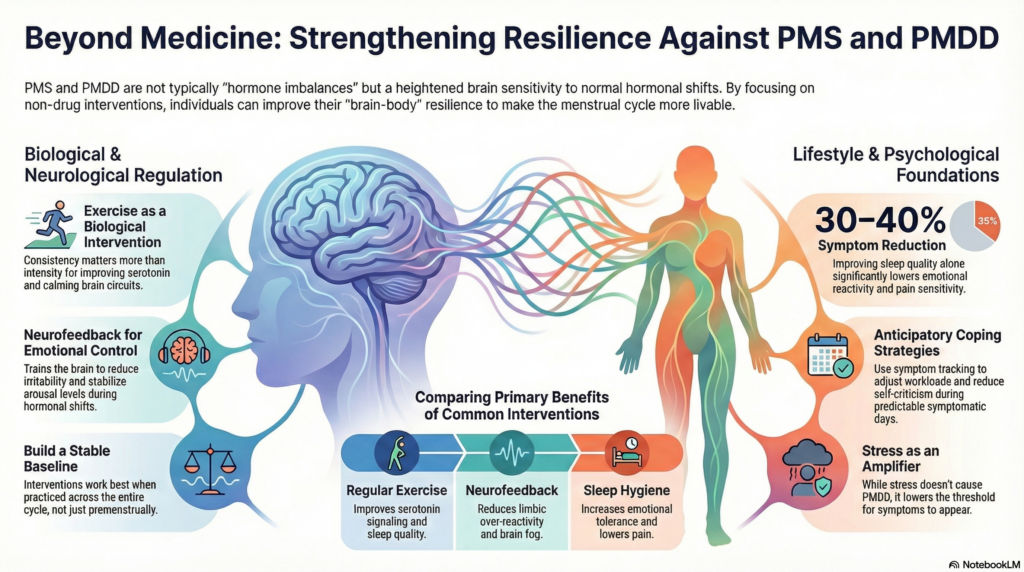
They are conditions of heightened brain sensitivity to normal hormonal changes, particularly in the luteal phase. The goal of non-drug management is not to eliminate the cycle—but to improve resilience and regulation across it.
1. Exercise: the most underrated treatment
Exercise is not a lifestyle “add-on” for PMS/PMDD. It is a biological intervention.
Regular physical activity improves:
-
Serotonin signalling
-
GABAergic inhibition (calming circuits)
-
Stress hormone regulation
-
Sleep quality
-
Emotional reactivity
What kind of exercise works best?
Consistency matters more than intensity.
Effective options include:
-
Brisk walking
-
Cycling or swimming
-
Strength training
-
Yoga and pilates
-
Moderate aerobic workouts
The biggest benefit comes when exercise is regular across the entire cycle, not only during the premenstrual phase. This creates a more stable baseline, so the luteal-phase dip is less dramatic.
A common clinical observation:
Women who exercise regularly still feel premenstrual changes—but they cope better and recover faster.
2. Neurofeedback: training emotional regulation
Neurofeedback is particularly well-suited for PMS and PMDD because these are state-dependent disorders—symptoms emerge when regulation systems are stressed.
How neurofeedback helps
Using EEG-based feedback, neurofeedback trains the brain to:
-
Reduce limbic over-reactivity (irritability, emotional surges)
-
Improve prefrontal control (impulse and emotion regulation)
-
Stabilise arousal levels
-
Improve stress recovery
Over time, this leads to greater emotional flexibility, especially during the luteal phase.
What changes clinically?
Women often report:
-
Less irritability and anger
-
Reduced anxiety
-
Better emotional control
-
Improved sleep
-
Less “brain fog” before periods
Neurofeedback does not change hormones.
It changes how the brain responds to hormonal shifts.
3. Sleep: the silent amplifier
Poor sleep worsens PMS and PMDD more than most people realise.
Sleep deprivation:
-
Lowers emotional tolerance
-
Increases pain sensitivity
-
Amplifies irritability and anxiety
-
Disrupts serotonin and stress systems
Simple but powerful steps include:
-
Fixed sleep and wake times
-
Reducing late-night screen exposure
-
Avoiding caffeine late in the day
-
Protecting sleep especially in the premenstrual week
For many women, improving sleep alone reduces symptom severity by 30–40%.
4. Psychological strategies: working with the cycle
PMS and PMDD are predictable. This predictability can be used therapeutically.
Helpful approaches include:
-
Symptom tracking across cycles
-
Anticipatory coping (adjusting workload, expectations)
-
Cognitive strategies to manage negative thought spirals
-
Reducing self-criticism during symptomatic days
Structured therapies such as CBT can help, but even simple psychoeducation—understanding that symptoms are cyclical and temporary—reduces distress and loss of control.
5. Nutrition and body regulation
While no diet “cures” PMS or PMDD, some patterns help reduce vulnerability:
-
Regular meals to stabilise blood sugar
-
Adequate protein intake
-
Reducing excessive caffeine and alcohol
-
Staying hydrated
Magnesium-rich foods and balanced nutrition may help with physical symptoms and fatigue, though effects are modest and individual.
6. Stress management: not optional
Chronic stress does not cause PMDD—but it lowers the threshold at which symptoms appear.
Effective strategies include:
-
Breathing exercises
-
Mindfulness or body-based relaxation
-
Reducing unnecessary commitments premenstrually
-
Learning to pause rather than push through
The aim is not perfect calm, but faster recovery from stress.
Who benefits most from non-medication approaches
Non-pharmacological strategies work best when:
-
Symptoms are mild to moderate
-
There is insight and motivation
-
Emotional reactivity is a key feature
-
Medication is poorly tolerated or not preferred
In more severe PMDD, these approaches still matter—but may work best alongside medication, not instead of it.
The core idea
Managing PMS and PMDD without medicines is not about “natural fixes.”
It is about strengthening regulation—in the brain, body, and daily rhythms—so hormonal changes no longer take control.
Exercise builds resilience.
Neurofeedback improves emotional regulation.
Sleep and stress management reduce amplification.
Together, they don’t erase the cycle.
They make it livable.
About the author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall)
Dr. Srinivas works extensively with PMS, PMDD, mood disorders, anxiety disorders, and stress-related conditions. His approach emphasises brain-based self-regulation, lifestyle stabilisation, and careful use of treatments—helping patients improve functioning without unnecessary long-term medication.
✉ srinivasaiims@gmail.com
📞 +91-8595155808