Antidepressants for Premenstrual Symptoms: Why Continuous Treatment Often Works Better
 Premenstrual symptoms are common. Premenstrual distress is not.
Premenstrual symptoms are common. Premenstrual distress is not.
For a subset of women, the days before menstruation bring predictable, cyclical, and impairing emotional and physical symptoms that disrupt work, relationships, and self-confidence. This spectrum ranges from Premenstrual Syndrome (PMS) to the more severe Premenstrual Dysphoric Disorder (PMDD).
Over the past few decades, one finding has remained remarkably consistent:
antidepressants—particularly SSRIs—can significantly reduce premenstrual symptoms.
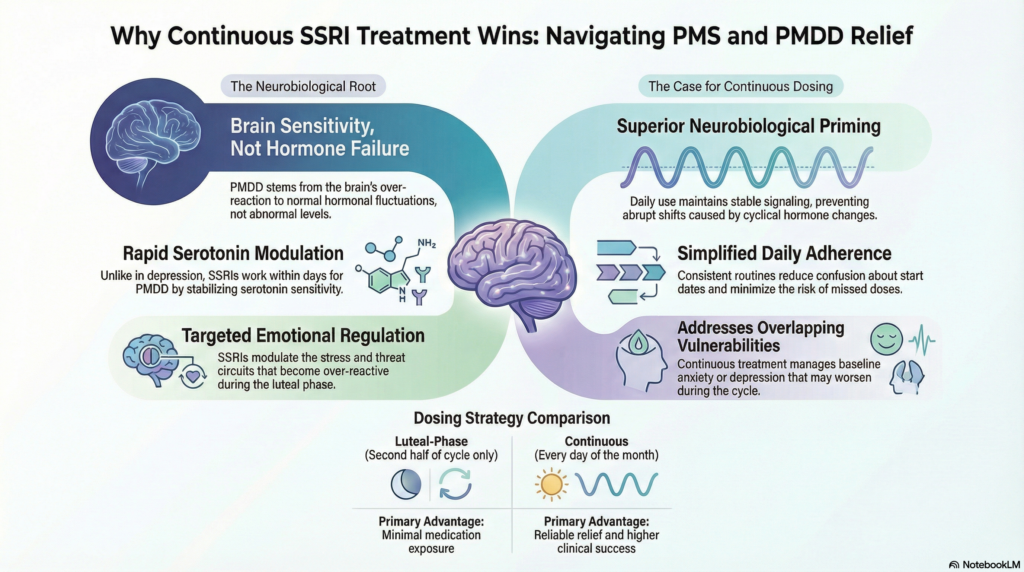
Even more interestingly, continuous daily treatment appears to be more effective than luteal-phase–only dosing for many women.
Let’s unpack why.
Understanding PMS and PMDD: not a hormone imbalance problem
PMS and PMDD are not caused by abnormal hormone levels.
Estrogen and progesterone are usually within normal ranges.
The issue lies in how the brain responds to normal hormonal fluctuations, particularly during the luteal phase (the second half of the menstrual cycle).
Key features include:
-
Heightened emotional reactivity
-
Increased anxiety, irritability, or low mood
-
Reduced stress tolerance
-
Somatic symptoms such as fatigue, bloating, and pain
This pattern points toward neurotransmitter sensitivity, not endocrine failure.
Why antidepressants work for premenstrual symptoms
SSRIs (selective serotonin reuptake inhibitors) have a unique role here.
Unlike in depression—where antidepressants take weeks to work—in PMS and PMDD:
-
Symptom relief can occur within days
-
Even low doses may be effective
-
Benefits extend to emotional, behavioural, and physical symptoms
This rapid effect suggests SSRIs are modulating serotonin sensitivity, not simply correcting a “low serotonin” state.
Serotonin interacts closely with:
-
Progesterone metabolites (especially allopregnanolone)
-
Stress and threat circuits
-
Emotional regulation networks
In PMS/PMDD, these systems become over-reactive in the luteal phase. SSRIs appear to stabilise this response.
Continuous vs luteal-phase dosing: what’s the difference?
Two main prescribing strategies are used:
Luteal-phase dosing
-
Antidepressant is taken only in the second half of the cycle
-
Usually started after ovulation and stopped at menstruation
Continuous dosing
-
Antidepressant is taken every day throughout the cycle
Both approaches can work. However, evidence and clinical experience increasingly suggest that continuous dosing is often more effective, especially in real-world settings.
Why continuous treatment often works better
Several reasons explain this advantage.
First, symptoms often begin earlier than expected.
Many women experience emotional changes before they clearly enter the luteal phase, making timing difficult.
Second, neurobiological priming matters.
Continuous SSRI use maintains stable serotonin signalling, preventing the abrupt sensitivity shifts that occur with cyclical hormone changes.
Third, adherence is simpler.
Daily medication avoids confusion about when to start or stop, reducing missed doses and partial treatment.
Finally, many women with PMS or PMDD also have:
-
Underlying anxiety disorders
-
Recurrent depression
-
Stress-related symptoms that are not strictly cyclical
In these cases, continuous treatment addresses both baseline vulnerability and cyclical worsening.
Does luteal-phase dosing still have a role?
Yes—especially when:
-
Symptoms are strictly limited to the premenstrual period
-
The woman prefers minimal medication exposure
-
There is good cycle regularity and reliable symptom tracking
However, luteal-phase dosing tends to be less forgiving. Timing errors, stress, sleep disruption, or cycle variability can all reduce effectiveness.
Which antidepressants are typically used?
SSRIs are the mainstay, including:
-
Low to moderate doses
-
Often lower than those used for major depression
The goal is symptom control, not emotional blunting. Dose adjustments are guided by response, tolerability, and functional improvement.
What about side effects?
At the doses used for PMS/PMDD:
-
Side effects are usually mild
-
Many women tolerate SSRIs well
-
Sexual side effects and emotional flattening are less common at lower doses but should still be discussed openly
Importantly, treatment should always be reviewed periodically, not continued indefinitely by default.
Medication is not the whole story
Antidepressants work best when combined with:
-
Psychoeducation (understanding the cyclical nature of symptoms)
-
Stress regulation strategies
-
Sleep stabilisation
-
Cognitive and behavioural techniques
For some women, lifestyle and psychological interventions may be sufficient. For others, medication provides the neurobiological stability that makes those strategies possible.
The take-home message
PMS and PMDD are real, biologically grounded conditions—not a failure of willpower or resilience.
Antidepressants, particularly SSRIs, can significantly reduce premenstrual symptoms.
While luteal-phase dosing can be effective, continuous treatment often provides more consistent, reliable relief, especially in women with severe symptoms or overlapping anxiety and mood vulnerability.
Treatment should always be individualised, collaborative, and reviewed over time.
About the author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall)
Dr. Srinivas works extensively with mood disorders, anxiety disorders, perinatal and reproductive mental health, and stress-related conditions. His clinical approach integrates neuroscience, careful pharmacology, and psychotherapy to help patients achieve stability without over-medicalisation.
✉ srinivasaiims@gmail.com
📞 +91-8595155808