Dementia Is Not Diagnosed by Memory Tests Alone – A Modern Review of Computerised Assessment and Cognitive Remediation in Neurocognitive Disorders
 One of the most persistent myths in dementia care is this:
One of the most persistent myths in dementia care is this:
“If someone fails a memory test, they have dementia.
If they pass a memory test, they don’t.”
This belief is wrong — and clinically dangerous.
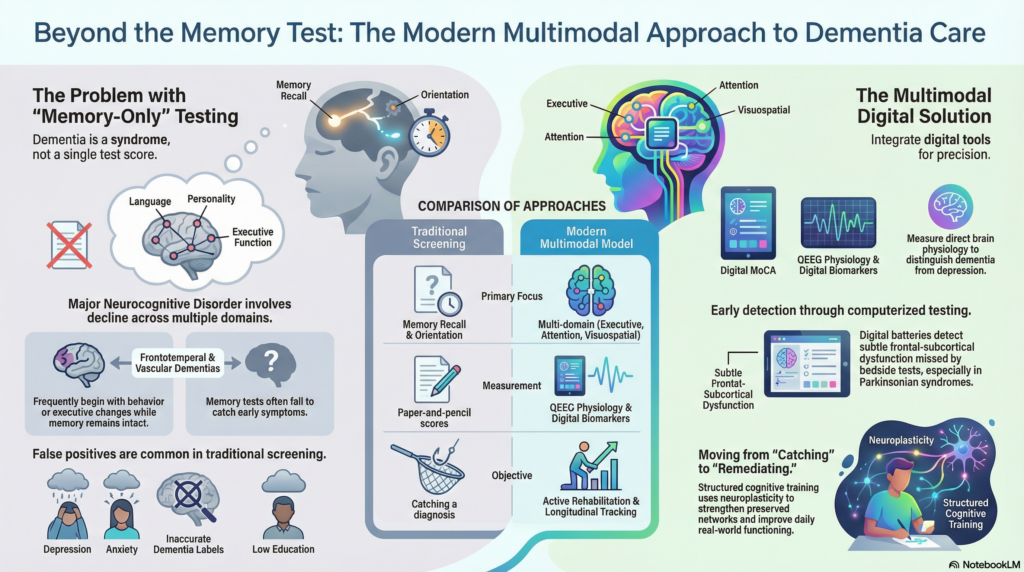
In modern psychiatry and neurology, dementia (major neurocognitive disorder) is not diagnosed on the basis of memory tests alone. Memory is only one domain of cognition. Many neurocognitive disorders begin with problems in attention, executive function, language, visuospatial ability, behaviour, or personality — long before memory clearly fails.
This is why contemporary dementia care has moved beyond bedside questioning and paper-and-pencil tests toward a multimodal model that integrates:
• computerised cognitive assessment
• quantitative brain-function measures (QEEG)
• longitudinal digital tracking
• and structured cognitive training and remediation
What Dementia Actually Means
Dementia, now termed Major Neurocognitive Disorder (NCD) in DSM-5, is defined by:
• a decline from a previous level of cognitive functioning
• impairment in one or more cognitive domains
• interference with independence in everyday life
The key words are decline, multiple domains, and functional impairment.
This immediately tells us something essential:
Dementia is not a single-test diagnosis.
It is a syndrome, not a score.
Why Memory Tests Alone Are Inadequate
Traditional dementia screening relies heavily on:
• memory recall tasks
• orientation questions
• naming objects
• copying figures
While useful, these tests suffer from four major limitations.
1) Many Dementias Do Not Begin With Memory Loss
In several common neurocognitive disorders, early memory can be relatively preserved.
Examples:
• Frontotemporal dementia → early personality and behaviour change
• Vascular dementia → slowed thinking and executive dysfunction
• Lewy body dementia → visuospatial deficits and attention fluctuation
• Parkinson’s disease dementia → executive dysfunction and attention
A patient may pass a basic memory test and still have a neurodegenerative disorder.
2) Depression, Anxiety, and Sleep Disorders Mimic Dementia
So-called “pseudodementia” is common.
Severe depression, anxiety, and insomnia can cause:
• poor concentration
• slowed thinking
• impaired recall
• disorganisation
These patients often fail memory tests but do not have dementia.
Relying only on memory scores creates false positives.
3) Education, Language, and Test Anxiety Distort Scores
Low education, illiteracy, sensory deficits, and anxiety during testing all reduce test performance.
This produces:
• false dementia diagnoses
• unnecessary panic
• inappropriate labelling
4) Single Test Scores Cannot Track Decline
Dementia is defined by progression over time.
A single score tells us nothing about:
• rate of decline
• stability
• treatment response
• functional trajectory
What Modern Dementia Diagnosis Actually Requires
A valid diagnosis of dementia or major neurocognitive disorder requires integration of:
• clinical history and decline pattern
• functional impairment
• multi-domain cognitive testing
• mood and sleep evaluation
• medical and medication review
• brain imaging and laboratory tests when indicated
• longitudinal follow-up
Computerised tools exist to strengthen — not replace — this clinical process.
Digital MoCA: A Screening Tool, Not a Diagnosis
The Montreal Cognitive Assessment (MoCA) is one of the most sensitive screening tools for:
• mild cognitive impairment
• early dementia
• executive dysfunction
• attention deficits
Unlike older tests, MoCA samples:
• attention
• executive function
• language
• visuospatial ability
• abstraction
• memory
• orientation
This makes it far superior to memory-heavy tools such as the MMSE.
Why Digital MoCA Is a Major Advance
Digitised MoCA versions add important advantages:
• standardised administration
• automated scoring
• reduced examiner bias
• precise timing
• longitudinal comparison
• improved patient comfort
Most importantly, digital MoCA converts a one-time screening tool into a longitudinal cognitive biomarker.
But MoCA alone still does not diagnose dementia.
It only tells us whether cognitive performance is abnormal.
QEEG: Measuring Brain Dysfunction Directly
While cognitive tests measure performance, QEEG (Quantitative EEG) measures brain physiology.
QEEG analyses electrical brain activity to detect abnormalities in:
• dominant frequency
• spectral slowing
• coherence and connectivity
• network organisation
Typical QEEG Findings in Dementia
Well-replicated findings include:
• increased delta and theta power
• reduced alpha rhythm
• frontal-temporal disconnection
• reduced interhemispheric coherence
• network-level disorganisation
These abnormalities often appear before severe cognitive symptoms develop.
What QEEG Adds Clinically
QEEG helps clinicians:
• distinguish dementia from depression-related cognitive impairment
• identify neurodegenerative vs functional syndromes
• detect early network dysfunction
• monitor disease progression
• support difficult diagnoses
QEEG does not diagnose dementia on its own.
It provides biological evidence that complements cognitive testing and clinical evaluation.
Computerised Executive-Function and Attention Testing
Many dementias begin with executive dysfunction, not memory loss.
Computerised batteries can assess:
• processing speed
• divided attention
• working memory
• inhibition control
• cognitive flexibility
• reaction-time variability
These tools detect subtle frontal-subcortical dysfunction that bedside tests often miss.
They are especially valuable in:
• vascular dementia
• frontotemporal dementia
• Parkinsonian syndromes
• early-onset dementias
Why Integration Matters More Than Any Single Test
The modern approach to dementia assessment is multimodal.
A meaningful evaluation integrates:
• clinical history and decline pattern
• functional impairment
• digital MoCA
• executive-function testing
• QEEG biomarkers
• mood and sleep screening
• longitudinal follow-up
This creates a cognitive–brain phenotype, not just a test score.
From Assessment to Intervention: Cognitive Training and Remediation
Assessment without intervention is incomplete care.
Once a patient’s cognitive profile is established, modern dementia care increasingly includes structured cognitive training and cognitive remediation.
These interventions aim not to “cure” dementia, but to:
• strengthen preserved cognitive networks
• slow functional decline
• improve everyday performance
• enhance quality of life
• reduce caregiver burden
Clinic-Based Cognitive Training
In-clinic cognitive training allows:
• supervised, structured cognitive exercises
• individualised difficulty progression
• real-time feedback
• targeting of specific impaired domains
These sessions may focus on:
• attention and concentration
• working memory
• executive function
• processing speed
• visuospatial skills
Clinic-based training is especially useful in:
• mild cognitive impairment
• early dementia
• post-stroke cognitive impairment
• depression-related cognitive dysfunction
Home-Based Digital Cognitive Training
Home-based cognitive training extends therapy beyond the clinic.
Using tablet- or computer-based platforms, patients can engage in:
• daily or weekly cognitive exercises
• structured memory and attention tasks
• adaptive difficulty training
• gamified cognitive workouts
This allows:
• high-frequency stimulation of cognitive networks
• continuity of care
• greater accessibility for elderly patients
• long-term engagement
Progress can be monitored remotely and adjusted clinically.
Cognitive Remediation: A Neuroplasticity-Based Approach
Cognitive remediation is a structured, neuroscience-informed intervention that aims to:
• improve impaired cognitive processes
• teach compensatory strategies
• strengthen functional brain networks
• translate cognitive gains into real-world functioning
It combines:
• repetitive cognitive training
• strategy coaching
• psychoeducation
• behavioural adaptation
Cognitive remediation is particularly valuable in:
• mild cognitive impairment
• early dementia
• vascular cognitive impairment
• post-stroke syndromes
• depression-related cognitive dysfunction
Why Cognitive Training Matters in Dementia Care
Cognitive training and remediation:
• improve attention and processing speed
• enhance executive function
• slow decline in early dementia
• improve daily functioning
• increase patient confidence
• reduce caregiver stress
They transform dementia care from pure diagnosis into active rehabilitation.
A Humane Point That Matters
Traditional memory testing often feels humiliating.
Patients feel judged.
Families feel frightened.
Everyone feels uncertain.
Digital assessment and structured cognitive training can be delivered in a way that feels:
• respectful
• calm
• collaborative
• empowering
The goal is not to “catch dementia.”
The goal is to understand what the brain is doing — and what can still be done to help it.
Final Reflection
Dementia is not diagnosed by memory tests alone.
It is diagnosed by understanding decline, domains, dysfunction, and progression.
MoCA, QEEG, and computerised cognitive tools do not replace clinical judgment.
They rescue it from guesswork.
Cognitive training and remediation then convert diagnosis into action.
That is what modern dementia care looks like.
About The Author
Dr. Srinivas Rajkumar T, MD (AIIMS, New Delhi), DNB
MBA (Health & Hospital Systems Management), BITS Pilani
Consultant Psychiatrist & Neurofeedback Specialist
Founder – Mind & Memory Clinic
Consultation Locations:
Mind & Memory Clinic – Apollo Clinic Velachery (Opposite Phoenix Mall)
Apollo Clinic, Tansi Nagar
MGM Malar Hospital, Adyar
Kumar Hospital, Chromepet
✉ srinivasaiims@gmail.com
📞 +91-8595155808
Special Services:
• Computerised dementia assessment in Chennai
• Digital MoCA screening
• QEEG-based brain-function analysis
• Executive-function and attention profiling
• Fast-track memory clinic services
• Clinic-based cognitive training
• Home-based digital cognitive training
• Cognitive remediation therapy
• Longitudinal cognitive monitoring