Behaviour Changes in Elderly with Dementia: What Caregivers Need to Know
 One of the most difficult parts of caring for a person with dementia is behaviour, not memory loss.
One of the most difficult parts of caring for a person with dementia is behaviour, not memory loss.
While forgetting names or events is expected, behaviour changes are what exhaust caregivers emotionally and physically.
It is important to understand this clearly:
These behaviours are part of the illness.
They are not deliberate, and they are not the person’s fault.
What Kind of Behaviour Changes Can Happen?
A person with dementia may show a wide range of behavioural and psychological symptoms, including:
-
restlessness, pacing, or wandering
-
irritability, anger, shouting, or verbal aggression
-
repeated questioning or calling out
-
fear, suspicion, or false beliefs (delusions)
-
seeing or hearing things that are not present (hallucinations)
-
social withdrawal or loss of interest
-
disinhibition (saying or doing socially inappropriate things)
-
resistance to care such as bathing or dressing
-
disturbed sleep, night-time confusion, or reversal of sleep–wake cycle
To caregivers, this can feel frightening or embarrassing, and sometimes even frighteningly “out of character”.
In reality, the brain has changed, not the person’s intentions or values.
Hallucinations and Delusions: Especially Distressing but Common
Some people with dementia may:
-
see people, animals, or shadows that are not there
-
believe someone is stealing from them
-
think family members are strangers or impostors
-
feel that others are trying to harm or deceive them
These experiences feel very real to the person.
Arguing or trying to prove them wrong usually increases fear and agitation.
Reassurance, calm presence, and medical evaluation are far more helpful.
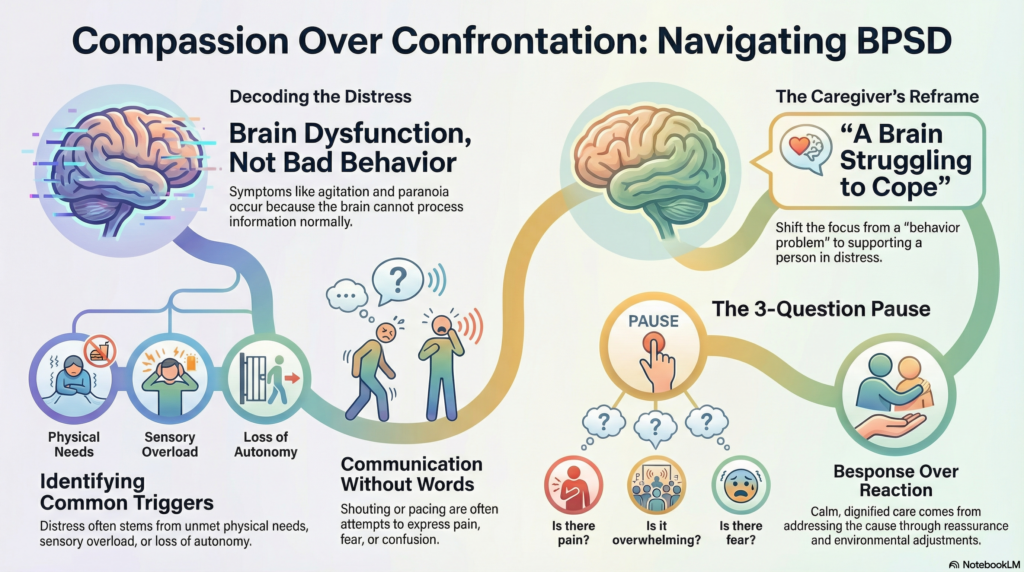
Why Do These Behaviours Happen?
In dementia, the brain struggles to correctly understand and interpret reality.
Behavioural symptoms often arise from:
-
brain changes affecting perception, judgment, and impulse control
-
unmet physical needs
(pain, infection, constipation, hunger, poor sleep) -
confusion or sensory overload
(noise, crowds, unfamiliar environments) -
fear due to misinterpretation
(misreading faces, sounds, shadows, or intentions) -
loss of control and autonomy
(being rushed, corrected, or forced)
When the brain cannot explain distress in words, it shows distress through behaviour.
Behaviour Is Often Communication Without Words
A helpful way to think about behaviour is this:
Behaviour is communication when language no longer works.
The person may be trying to express:
-
“I am frightened”
-
“I am uncomfortable”
-
“I don’t understand what is happening”
-
“I feel threatened or confused”
They are not trying to create trouble.
What Should Caregivers Do First?
Before reacting to difficult behaviour, pause and ask:
-
Could there be pain, illness, or discomfort?
-
Are they overwhelmed by noise or activity?
-
Has the routine changed suddenly?
-
Are they frightened by something they misinterpreted?
Very often, reducing distress reduces behaviour.
What Commonly Makes Behaviour Worse?
Some natural reactions increase distress:
-
arguing or correcting false beliefs
-
insisting on logic
-
rushing care
-
scolding or threatening
These reactions come from exhaustion—but they increase fear in a confused brain.
A Simple Mental Shift That Helps
Keep this sentence close:
“This is not bad behaviour.
This is a brain illness expressing itself.”
Once caregivers accept this:
-
anger reduces
-
guilt reduces
-
care becomes calmer and safer
Care shifts from control to reassurance, structure, and dignity.
A Note From the Clinician
Over the years, I have guided thousands of caregivers through these exact challenges—helping families manage behavioural symptoms such as agitation, hallucinations, delusions, and disinhibition using a balanced, individualised approach that includes:
-
careful use of medicines when truly needed
-
non-drug strategies and environmental modifications
-
clear explanation of why behaviours occur
-
emotional support and burnout prevention for caregivers
When caregivers understand what is happening in the brain, they feel less helpless and more confident—and patients are calmer, safer, and more comfortable.
About the Author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall)
✉ srinivasaiims@gmail.com
📞 +91-8595155808