Psychiatric Medicines During Pregnancy: A Clear, Calm Guide for Patients and Families
 Pregnancy is often portrayed as a purely joyful phase. Clinically, it is also a period of major neurobiological, hormonal, and psychological change. For many women, existing psychiatric conditions may recur, worsen, or newly emerge during pregnancy.
Pregnancy is often portrayed as a purely joyful phase. Clinically, it is also a period of major neurobiological, hormonal, and psychological change. For many women, existing psychiatric conditions may recur, worsen, or newly emerge during pregnancy.
One of the most common—and understandable—concerns is this:
“Are psychiatric medicines safe during pregnancy?”
The honest answer is not black or white. It is nuanced, evidence-based, and deeply individual.
First principles: why this decision matters
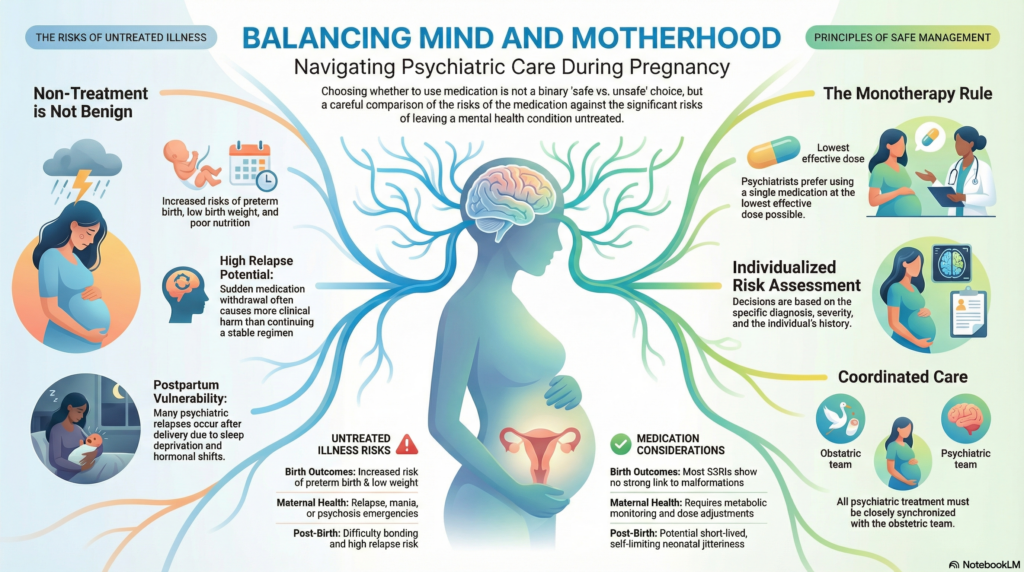
Untreated psychiatric illness during pregnancy is not benign.
Moderate to severe depression, anxiety, bipolar disorder, OCD, or psychosis can increase the risk of:
-
Poor self-care and nutrition
-
Sleep deprivation and stress physiology
-
Substance use or medication non-adherence
-
Preterm birth and low birth weight
-
Postpartum relapse and bonding difficulties
So the real clinical question is not medication vs no medication.
It is risk of treatment vs risk of untreated illness.
General rules psychiatrists follow in pregnancy
Across conditions and medications, a few principles guide safe practice:
-
Use medication only when clinically indicated
-
Prefer monotherapy over combinations
-
Use the lowest effective dose, not subtherapeutic dosing
-
Avoid abrupt stopping of long-term medication
-
Avoid first-trimester changes unless necessary
-
Coordinate care with the obstetric team
Stability matters. Sudden medication withdrawal often causes more harm than continuation.
Antidepressants in pregnancy
Antidepressants—especially SSRIs—are the most commonly used psychiatric medications in pregnancy.
What we know:
-
Most SSRIs have no strong association with major congenital malformations
-
The absolute risk, when present, is small
-
Relapse rates are high when effective antidepressants are stopped abruptly
Some SSRIs have better reproductive safety data than others, which is why psychiatrists often choose rather than avoid medication.
Late-pregnancy exposure may rarely be associated with:
-
Transient neonatal adaptation symptoms (jitteriness, mild respiratory issues)
-
These are usually self-limiting and short-lived
OCD and anxiety disorders
OCD and anxiety often worsen during pregnancy and postpartum, driven by threat sensitivity and hormonal shifts.
Medication may be indicated when:
-
Intrusive thoughts are severe or distressing
-
Compulsions interfere with daily functioning
-
CBT alone is insufficient or unavailable
Medication plus psychotherapy—especially CBT or ERP—often provides the best outcome.
Mood stabilisers and bipolar disorder
This is one of the highest-risk areas in perinatal psychiatry.
-
Bipolar disorder has a very high relapse risk during pregnancy and postpartum
-
Some mood stabilisers carry known teratogenic risks
-
Others may be used cautiously with monitoring
Stopping medication in bipolar disorder can precipitate:
-
Severe depression
-
Mania or psychosis
-
Postpartum psychiatric emergencies
Management here must be individualised and specialist-led.
Antipsychotics during pregnancy
Antipsychotics are sometimes necessary for:
-
Schizophrenia
-
Bipolar disorder
-
Severe depression with psychotic features
Current evidence suggests many modern antipsychotics do not significantly increase major malformation risk, though metabolic monitoring is important.
The greater danger is often relapse of psychosis, which can endanger both mother and fetus.
What about the first trimester?
The first trimester is when organ development occurs, so:
-
Medication changes are avoided unless clearly needed
-
If a woman is already stable on medication, continuation is often safer than switching
-
Planned pregnancies allow pre-conception optimisation, which is ideal
Unplanned pregnancies are common. The priority then becomes calm risk assessment, not panic-driven discontinuation.
After delivery: thinking ahead
Pregnancy planning must always include the postpartum period, which is a time of:
-
Sleep deprivation
-
Hormonal withdrawal
-
High relapse risk
Many psychiatric relapses occur after delivery, not during pregnancy. Medication decisions should anticipate this phase, especially when breastfeeding is planned.
The most important message
There is no single “safe” or “unsafe” psychiatric medicine in pregnancy.
There is only:
-
A specific diagnosis
-
A specific severity
-
A specific medication
-
A specific person
Good perinatal psychiatry is about measured decisions, not fear-based ones.
About the author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall)
Dr. Srinivas works extensively with perinatal mental health conditions, including depression, anxiety disorders, OCD, and bipolar disorder. His approach balances scientific evidence with clinical judgment, helping families make informed, calm decisions during pregnancy and beyond.
✉ srinivasaiims@gmail.com
📞 +91-8595155808