Dementia: A Practical Guide for Caregivers
Behavioural symptoms, communication, burnout prevention, and dignity-focused care
Caring for a person with dementia is not only about memory loss. It is about navigating changed behaviour, altered emotions, disrupted communication, and gradual role reversal—often while the caregiver’s own life quietly shrinks around the illness.
This guide is written for caregivers who want clarity without complexity, and science without coldness.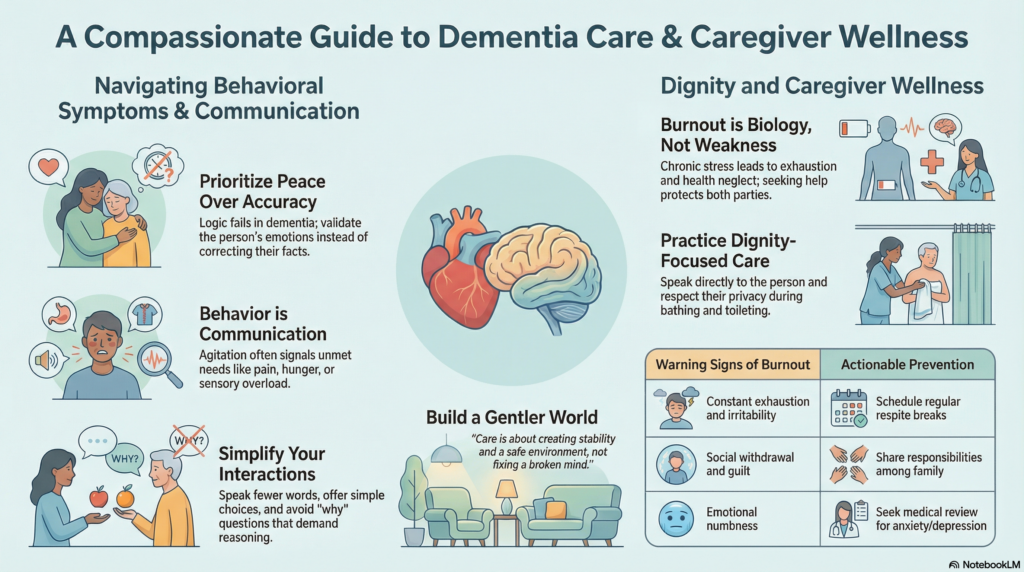
Dementia is not just memory loss
Most people associate dementia with forgetting names or repeating questions. But what strains families the most are behavioural and psychological symptoms, often called BPSD.
These may include:
-
Agitation, restlessness, or pacing
-
Irritability or sudden anger
-
Suspicion, fear, or false beliefs
-
Sleep–wake reversal
-
Apathy or emotional withdrawal
These behaviours are not intentional. They are expressions of a brain struggling to interpret the world.
The goal of caregiving is not to “correct” the person—but to reduce distress.
Understanding behavioural symptoms: what’s really happening?
Behavioural symptoms usually arise from one or more of the following:
-
Unmet needs
Pain, hunger, constipation, infection, poor sleep, or sensory overload. -
Cognitive mismatch
The environment demands skills the brain no longer has—time awareness, judgment, sequencing. -
Emotional memory remains intact
Even when factual memory fades, the feeling of fear, shame, or safety remains strong.
Before reacting to behaviour, pause and ask:
“What might they be trying to communicate?”
This simple shift prevents many confrontations.
Communication: stop arguing with the illness
One of the hardest lessons for caregivers is this:
Logic does not work in dementia.
Correcting, confronting, or proving facts often escalates distress.
Principles of dementia-friendly communication
-
Slow down: Speak fewer words, not louder words
-
Validate emotion, not facts
“I see you’re worried” works better than “That’s not true” -
Offer choices, not commands
“Would you like tea or water?” instead of “Drink this” -
Avoid ‘why’ questions
They demand reasoning the brain can no longer perform
When a person insists on something untrue, ask:
“Is correcting this helping—or hurting?”
Peace is often more therapeutic than accuracy.
Managing common behavioural challenges
Agitation and restlessness
Often linked to anxiety, pain, or boredom.
Helpful strategies:
-
Gentle routine and predictability
-
Short walks or light physical activity
-
Soft music or familiar sounds
-
Checking for pain, urinary issues, constipation
Medication is not the first solution. Environment and reassurance matter more.
Sleep disturbances
Common due to circadian rhythm disruption.
Practical steps:
-
Daytime sunlight exposure
-
Avoid long daytime naps
-
Quiet evenings, dim lights after sunset
-
Consistent bedtime routine
Sedatives should be used cautiously and only under medical guidance.
Suspicion or paranoia
Arguing worsens fear.
Instead:
-
Reassure safety
-
Avoid validating false beliefs directly
-
Redirect attention gently
Example:
“I’ll stay with you. You’re safe.”
Dignity-focused care: the ethical core of caregiving
Dementia slowly strips away independence—but dignity must never be optional.
Dignity-focused care means:
-
Speaking to the person, not about them
-
Avoiding infantilising language
-
Respecting privacy during bathing and toileting
-
Including them in decisions at whatever level remains possible
Even in advanced stages, the person is still present—emotionally, relationally, humanly.
Caregiver burnout: the invisible crisis
Caregivers often minimise their own suffering:
“Others have it worse.”
“This is my duty.”
But burnout is not weakness—it is biology and chronic stress.
Warning signs include:
-
Constant exhaustion
-
Irritability or guilt
-
Emotional numbness
-
Social withdrawal
-
Health neglect
A burned-out caregiver cannot provide good care.
Preventing caregiver burnout (this is not selfish)
Burnout prevention is care planning, not indulgence.
Practical steps:
-
Scheduled respite, even short breaks
-
Sharing responsibility—no single caregiver should do everything
-
Clear role division among family members
-
Medical review when depression or anxiety emerges
Seeking help early protects both the caregiver and the patient.
When medications are needed
Medications may help when:
-
Behaviour causes harm or severe distress
-
Non-pharmacological measures fail
-
Sleep or agitation threatens safety
They should be:
-
Used at the lowest effective dose
-
Reviewed regularly
-
Never used simply for convenience
Good dementia care is not about sedation, but stability.
What good dementia care really looks like
Good care is not dramatic. It is quiet, repetitive, patient.
It looks like:
-
Reduced distress
-
Fewer confrontations
-
Safer routines
-
A caregiver who is still functioning as a human being
Dementia cannot yet be cured—but suffering can be reduced.
Final thought
Dementia care is not about fixing a broken mind.
It is about building a gentler world around a vulnerable brain.
Small changes, done consistently, matter more than heroic effort.
About the Author
Dr. Srinivas Rajkumar T, MD (AIIMS), DNB, MBA (BITS Pilani)
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall)
✉ srinivasaiims@gmail.com
📞 +91-8595155808