Introduction to Psychodermatology: Where the Mind Meets the Skin
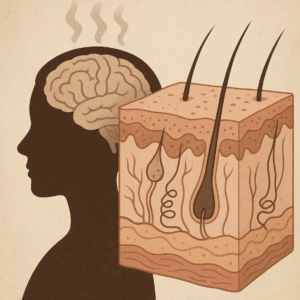
The skin is our most visible organ—our first line of defense, our interface with the world, and often, a mirror of what lies beneath. Just as emotions can flush our cheeks or stress can trigger a breakout, deeper psychological states often leave their marks on the skin. This intersection is the domain of psychodermatology, a field that bridges dermatology, psychiatry, and psychology.
What Is Psychodermatology?
Psychodermatology is the study of the two-way relationship between the mind and the skin. It recognizes that:
-
Psychological distress can trigger or worsen skin conditions.
-
Chronic skin disorders can in turn affect mood, self-esteem, and social functioning.
-
Some psychiatric conditions present primarily through the skin.
In short, it’s not just about treating rashes or lesions—it’s about seeing the person behind the skin and understanding the invisible burdens they carry.
Why Does It Matter?
Skin diseases are common, visible, and often stigmatizing. Patients with psoriasis, vitiligo, or acne may experience anxiety, depression, or even social withdrawal. Conversely, stress, trauma, or unresolved conflict can fuel flare-ups of eczema or urticaria. For clinicians, ignoring this connection risks incomplete care; for patients, it means carrying a double burden—both the physical condition and its psychological weight.
Pathways Linking Mind and Skin
The science behind psychodermatology rests on well-documented mechanisms:
-
Neuroendocrine system: Stress activates the hypothalamic-pituitary-adrenal (HPA) axis, releasing cortisol, which can worsen inflammatory skin diseases.
-
Immune system: Emotional states can alter immune responses, changing the course of conditions like psoriasis.
-
Behavioral patterns: Anxiety may lead to scratching, picking, or hair-pulling, perpetuating cycles of damage.
The Three Broad Categories
Clinicians often think of psychodermatology in three buckets:
-
Psychiatric conditions with skin symptoms (e.g., trichotillomania, delusional parasitosis).
-
Skin conditions worsened by psychological factors (e.g., psoriasis, acne, eczema).
-
Psychiatric sequelae of skin disorders (e.g., depression or body image distress due to visible skin disease).
This framework helps guide assessment and treatment, reminding us that skin and psyche are inseparable.
Looking Ahead
Psychodermatology is not a niche—it’s a growing necessity. With rising awareness of mental health, more patients and clinicians are ready to move beyond the “skin-deep” model of care. Multidisciplinary clinics, integrating dermatologists, psychiatrists, and psychologists, are already showing better outcomes.
Ultimately, psychodermatology invites us to listen closely: to the skin, to the mind, and to the stories that connect them.
Dr. Srinivas Rajkumar T
MD (Psychiatry), AIIMS New Delhi
Consultant Psychiatrist – Child, Adult & Geriatric Psychiatry
Apollo Clinic, Velachery, Chennai
📞 Contact/WhatsApp: 85951 55808