Insight in OCD: From Clarity to Conviction
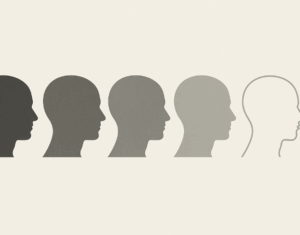 Not all patients with OCD see their thoughts and rituals in the same way. Some recognize them as irrational, others are only partly convinced, and a small minority believe their obsessions completely. This spectrum is called insight—and it has major implications for diagnosis, treatment, and prognosis.
Not all patients with OCD see their thoughts and rituals in the same way. Some recognize them as irrational, others are only partly convinced, and a small minority believe their obsessions completely. This spectrum is called insight—and it has major implications for diagnosis, treatment, and prognosis.
What Do We Mean by Insight?
Insight refers to how much a person recognizes that their obsessions and compulsions are excessive or unreasonable. It is not static—it can shift over time, and even vary across symptoms in the same individual.
The Brown Assessment of Beliefs Scale (BABS) is often used to measure it, scoring beliefs from “completely irrational” to “fully convinced.”
What the Data Show
In the Brazilian multicenter OCD study of over 1000 patients, the distribution of insight looked like this
-
Excellent insight: 31%
-
Good insight: 25%
-
Fair insight: 26%
-
Poor insight: 11%
-
Absent insight: 3%
Patterns worth noting:
-
Poorer insight was linked to earlier age of onset, greater symptom severity, and longer illness duration.
-
Insight didn’t differ significantly based on medication status at the time of evaluation.
Why Insight Matters Clinically
-
Differential Diagnosis
-
Patients with absent insight may appear delusional, risking misdiagnosis as psychosis. ICD-11 explicitly includes an insight specifier to prevent this error.
-
-
Treatment Engagement
-
Good insight patients often present earlier and adhere more readily to CBT or medication.
-
Poor/absent insight patients are more likely to resist therapy or drop out. They may need motivational strategies and stronger therapeutic alliances.
-
-
Severity Marker
-
Studies show poor insight correlates with more severe symptoms across dimensions—contamination, symmetry, aggression, hoarding, and more. Insight may be a proxy for illness severity.
-
The ICD-11 Step Forward
By including insight as a dimensional specifier, ICD-11 acknowledges the wide range of experiences within OCD. This change improves diagnostic accuracy and ensures clinicians don’t overlook patients at the more delusional end of the spectrum.
For psychiatry, this means a more nuanced approach—OCD is not simply about obsessions and compulsions, but also about how patients relate to those symptoms.
The Takeaway
Insight is not all-or-nothing. It is a sliding scale that shapes how patients experience OCD, how clinicians diagnose it, and how treatments succeed. Recognizing this dimension brings us closer to personalized care—and closer to understanding the lived reality of OCD.
About the Author
I’m Dr. Srinivas Rajkumar T, MD (AIIMS, New Delhi), Consultant Psychiatrist based in Chennai. Through my clinical practice and writing, I aim to make psychiatry more understandable and less intimidating.
📍 Mind and Memory Clinic, Apollo Clinic, Velachery, Chennai (Opp. Phoenix Mall)
📞 +91 85951 55808
🌐 srinivasaiims.com