🚼 Controlling Bedwetting in Children: What Every Parent Should Know
 Bedwetting (Nocturnal Enuresis) is common and stressful—not just for the child, but for the whole family. But here’s the good news: It’s treatable, and in most cases, temporary.
Bedwetting (Nocturnal Enuresis) is common and stressful—not just for the child, but for the whole family. But here’s the good news: It’s treatable, and in most cases, temporary.
Let’s understand how to tackle it with empathy and strategy.
🔍 What Is Enuresis?
-
Primary Enuresis: The child has never had a dry period for more than 6 months.
-
Secondary Enuresis: The child started bedwetting again after being dry for months. Often linked to stress or medical issues.
Usually diagnosed if:
-
Child is over 5 years old
-
Wetting occurs 2+ times a week
-
It lasts for 3 months or more
🚫 Myths vs Facts
| Myth | Fact |
|---|---|
| “The child is lazy.” | Most children cannot control it. It’s involuntary. |
| “It’s just psychological.” | Often there’s a delay in bladder control development or deep sleep. |
| “Punishing will fix it.” | Shame and scolding make it worse. |
🧠 Causes of Bedwetting
-
Delayed bladder maturity
-
Deep sleep (child doesn’t wake up with full bladder)
-
Family history (genetic)
-
Small bladder size
-
Constipation (presses bladder)
-
Stress or emotional changes
-
Urinary tract infection or diabetes (rare but must be ruled out)
🛠️ How to Manage and Control Bedwetting
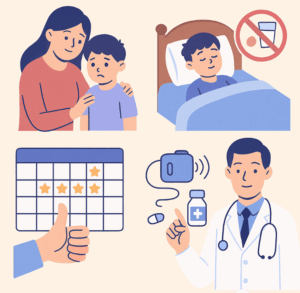
👨👩👧 1. Parenting Strategies
-
Reassure the child – never blame or punish.
-
Say: “It’s not your fault. You’re learning. We’ll fix it together.”
-
Encourage and reward dry nights, not punish wet ones.
🕰️ 2. Daily Routine Changes
-
Limit fluids 2 hours before bedtime.
-
Avoid caffeine or sugary drinks (even in milk).
-
Ensure child pees before sleep.
-
Use a bedwetting calendar to track progress.
🚽 3. Bladder Training
-
Encourage frequent bathroom breaks during the day.
-
Teach double voiding: pee, wait 10 minutes, pee again before bed.
-
Some children benefit from timed night wakings initially.
⏰ 4. Bedwetting Alarms
-
Most effective non-drug treatment (60–80% success).
-
Alarm sounds when it senses wetness, teaching the brain to wake up when the bladder is full.
💊 5. Medications (If needed and advised by a doctor)
-
Desmopressin (Minirin) – reduces urine production at night.
-
Imipramine – older option, used cautiously.
-
Best used short-term or for sleepovers, exams, etc.
🧪 When to Consult a Doctor
See a pediatrician or psychiatrist if:
-
Child is over 7 years and still bedwetting regularly
-
New onset after a long dry period
-
Daytime wetting, burning while peeing, or excessive thirst
-
Family stress or emotional issues are present
✅ What Not to Do
-
Don’t punish or shame the child.
-
Don’t overuse diapers—try absorbent mattress covers instead.
-
Don’t compare with siblings or other children.
💡 Final Word
Bedwetting is not your child’s fault. With the right mix of support, structure, and patience, most children overcome enuresis as their brain and bladder grow in sync.
Dr. Srinivas Rajkumar T, MBBS, MD (Psychiatry)
Consultant Psychiatrist
Apollo Clinics Velachery & Tambaram
🌱 Specialist in Child & Adolescent Mental Health
🌐 Visit: www.srinivasaiims.com
📞 For consults: Online & Offline appointments available