💊 Treatment of Bedwetting in Children: What Works and When to Seek Help
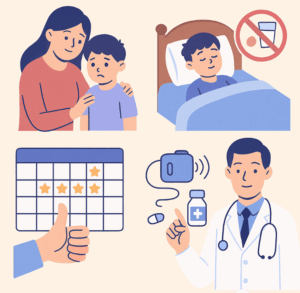
Bedwetting, or nocturnal enuresis, can feel frustrating for parents and deeply embarrassing for children. While reassurance and routines help many kids grow out of it, others need structured treatment. This article focuses on when and how to treat bedwetting medically and behaviorally.
📋 When Should You Start Treatment?
Most children achieve nighttime bladder control by age 5 to 7. If your child continues to wet the bed:
-
After age 7, regularly (more than 2 times a week)
-
If it causes distress, embarrassment, or affects sleepovers/school trips
-
If there is secondary enuresis (child was dry for months, then relapsed)
-
If there’s daytime wetting, constipation, or UTI symptoms
Then it’s time to consider active treatment.
🧠 The 3 Pillars of Enuresis Treatment
1. Behavioral Strategies
These are the first line of treatment.
-
Bladder training during the day (drink, hold, then void)
-
Double voiding before bedtime
-
Timed waking: Wake the child once 2–3 hours after sleep to urinate
-
Limit fluids 2 hours before bedtime
-
Reward systems: Stickers, praise for dry nights (not punishment for wet ones)
-
Use a bedwetting calendar to track progress and spot patterns
2. Enuresis Alarm Therapy
Most effective non-drug option with long-term benefit.
How It Works:
-
A sensor is attached to the child’s underwear or bedsheet
-
It rings or vibrates when it detects the first drop of urine
-
Over time, it conditions the brain to wake up when the bladder is full
Pros:
-
60–80% success with consistent use
-
No side effects
Cons:
-
Takes several weeks
-
Requires parental involvement and consistency
-
Not suited for families who cannot respond during the night
3. Medications
Reserved for older children, if alarms fail, or for short-term situations like school camps.
📌 a) Desmopressin (DDAVP)
-
Mimics antidiuretic hormone (reduces urine at night)
-
Quick results but risk of relapse if stopped abruptly
-
Taken as a melt or tablet, before bedtime
💡 Use with fluid restriction (no water 1 hour before or after) to avoid water retention and hyponatremia.
📌 b) Imipramine
-
A tricyclic antidepressant, reduces deep sleep and bladder contractions
-
Rarely used due to side effects (mood, heart rhythm)
📌 c) Oxybutynin or Tolterodine
-
For children with small bladder capacity or urgency
-
Used in combination with desmopressin or in daytime wetting cases
🔬 What to Check Before Starting Treatment
A pediatrician or psychiatrist may order:
-
Urine tests to rule out infections or diabetes
-
Bladder diaries to assess capacity and patterns
-
Abdominal X-rays or ultrasounds if constipation or anatomical issues are suspected
👨⚕️ When to Refer to a Specialist
Consider seeing a pediatric psychiatrist, urologist, or developmental pediatrician if:
-
Daytime symptoms are present
-
Child has emotional issues, anxiety, or attention problems
-
No response to 3–6 months of behavioral treatment
-
Enuresis is affecting school or social functioning
💬 What Children Need to Hear
“We’re working on this together. It’s not your fault. Many kids go through it. And there is treatment that can help.”
Shame delays help-seeking. Support speeds up recovery.
🧘 Final Thoughts
Bedwetting isn’t a willful behavior—it’s a developmental delay in nighttime bladder control. With the right tools, patience, and medical help when needed, most children grow out of it completely.
There’s no single solution, but a customized plan combining behavioral therapy, alarms, and medication (when needed) works for the vast majority.
Dr. Srinivas Rajkumar T, MBBS, MD (Psychiatry)
Consultant Psychiatrist
Apollo Clinics Velachery & Tambaram
🧒 Specialist in Child & Adolescent Psychiatry
🌐 Visit: www.srinivasaiims.com
📞 For appointments: Online & In-Person Consultations Available