Central Sensitisation: When the Nervous System Turns Up the Volume on Pain
 Pain is something we all experience — a cut, a sprain, or a headache tells us something is wrong. Normally, when the injury heals, the pain fades. But what happens when pain lingers, spreads across the body, or becomes severe without clear injury?
Pain is something we all experience — a cut, a sprain, or a headache tells us something is wrong. Normally, when the injury heals, the pain fades. But what happens when pain lingers, spreads across the body, or becomes severe without clear injury?
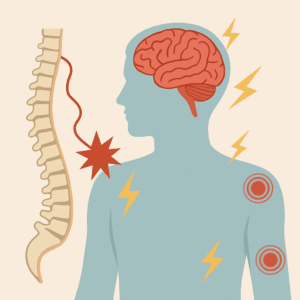
This is where the concept of central sensitisation comes in. It’s a scientific term that helps us understand why pain sometimes becomes amplified, persistent, and disabling.
What Is Central Sensitisation?
Central sensitisation is a process in which the central nervous system (the spinal cord and brain) becomes overly responsive to pain signals.
-
Normally: Pain signals travel from the site of injury → spinal cord → brain → sensation of pain.
-
In central sensitisation: The system gets “wound up,” making the pain volume knob stuck on high. Even minor triggers can feel unbearable.
The International Association for the Study of Pain (IASP) defines central sensitisation as “increased responsiveness of nociceptive neurons in the central nervous system to normal or subthreshold afferent input.”
Why Does It Happen?
Central sensitisation develops when pain pathways are repeatedly activated, causing long-term changes in the nervous system.
Key Mechanisms:
-
NMDA receptor activation → leads to exaggerated excitatory transmission.
-
Reduced inhibition → less GABA and glycine means less “braking” on pain signals.
-
Neuroinflammation → immune cells in the CNS release cytokines that further amplify pain.
-
Long-term potentiation → the spinal cord and brain “learn” to feel more pain, even without injury.
Clinical Features
People with central sensitisation often present with:
-
Widespread pain (not restricted to one site).
-
Disproportionate pain (severe distress despite minimal findings).
-
Allodynia (pain from normally non-painful stimuli, like touch or mild pressure).
-
Hyperalgesia (exaggerated pain response to a painful stimulus).
-
Overlap with fatigue, sleep problems, and emotional distress.
Conditions Linked to Central Sensitisation
Research has connected central sensitisation to many chronic pain syndromes, including:
-
Fibromyalgia
-
Vulvodynia
-
Plantar fasciitis with widespread pain patterns
-
Chronic low back pain
-
Temporomandibular joint disorders
-
Tension-type headaches and migraines
-
Irritable bowel syndrome
Why It Matters
For patients, central sensitisation explains why:
-
Pain feels real, even when scans or tests look normal.
-
Pain can be widespread and unpredictable.
-
Usual painkillers (like NSAIDs or opioids) often don’t work well.
For clinicians, it highlights the need for central modulation approaches, not just peripheral/local interventions.
Treatment Approaches
Since central sensitisation is about the nervous system being “too sensitive,” treatment focuses on calming and retraining the system.
1. Medications
-
SSRIs and SNRIs (e.g., Fluoxetine, Duloxetine, Venlafaxine) → improve serotonin and norepinephrine signaling, reducing pain amplification.
-
Gabapentinoids (Pregabalin, Gabapentin) → dampen excitatory neurotransmission.
-
Tricyclic antidepressants (low-dose Amitriptyline, Nortriptyline) → improve sleep and pain thresholds.
2. Non-Pharmacological
-
Cognitive Behavioral Therapy (CBT) → helps reduce pain catastrophising and improve coping.
-
Physiotherapy & Graded Exercise → gentle, paced activity retrains the nervous system.
-
Mind–Body Approaches → mindfulness, yoga, relaxation techniques lower nervous system hyperarousal.
-
Sleep optimization → crucial in resetting pain sensitivity.
Explaining to Patients: A Simple Analogy
You can think of central sensitisation as a smoke alarm that has become too sensitive.
-
Normally, it rings when there’s a fire.
-
But in central sensitisation, it rings loudly even when you just make toast.
-
The goal of treatment is to reset the alarm system so it only goes off when truly needed.
Key Takeaway
Central sensitisation is not “imaginary pain” — it’s a real neurobiological process where the nervous system amplifies pain. Recognising it helps patients understand their condition better and allows doctors to design effective treatments aimed at modulating the brain and spinal cord, not just the body part in pain.
By targeting both mind and body, patients can move from being trapped in pain to regaining function and quality of life.
📍 This article is part of our ongoing patient and clinician education series on chronic pain.
Dr. Srinivas Rajkumar T, MD (AIIMS, New Delhi)
Consultant Psychiatrist
Apollo Clinic, Velachery, Chennai
📞 8595155808