Myths, Misuse, and Mental Health – Conversations We Need to Have
Challenging stigma, clearing confusion, and changing the narrative
🚫 Why We Must Talk About It
Behind every untreated case of opioid addiction lies silence.
Silence born out of shame, misinformation, and fear.
Even today, in 2025, myths around opioid use and addiction block access to care, delay help-seeking, and fuel avoidable deaths. It’s time to set the record straight—because lives depend on it.
🧨 Common Myths and the Truth
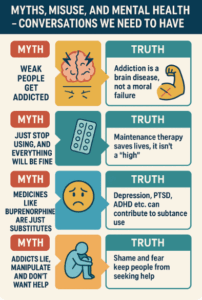
❌ Myth 1: “Only weak people get addicted.”
✅ Truth: Addiction is a brain disease, not a moral failure. It affects neuroplasticity, impulse control, and the stress system.
❌ Myth 2: “Just stop using and everything will be fine.”
✅ Truth: Sudden withdrawal can be dangerous, painful, and trigger severe depression or relapse. Recovery requires structured, stepwise support.
❌ Myth 3: “Medicines like buprenorphine are just substitutes.”
✅ Truth: Maintenance therapy is like insulin for diabetes. It reduces relapse risk, improves function, and saves lives. It’s not a “high”—it’s a bridge to stability.
❌ Myth 4: “Mental health has nothing to do with addiction.”
✅ Truth: Depression, trauma, anxiety, and ADHD often co-exist with addiction. Ignoring one while treating the other leads to failure.
❌ Myth 5: “Addicts lie, manipulate, and don’t want help.”
✅ Truth: Many people in active use feel shame, fear, and helplessness. They want help, but don’t know how to ask or where to go.
🧠 Mental Health and Opioid Use: A Two-Way Street
| Mental Health Issue | Role in Opioid Use |
|---|---|
| Depression | Self-medication with opioids |
| PTSD/Trauma | Escaping emotional pain |
| ADHD | Higher impulsivity and novelty-seeking |
| Personality disorders | Difficulty with emotional regulation |
🗣️ Conversations We Must Start Having
-
With families:
“Addiction is not about love or discipline—it’s about rewiring the brain. Support without enabling.” -
In workplaces and schools:
“Mental health screening and early education can prevent escalation.” -
Among clinicians:
“We need to move from policing to partnering. Use science, not stigma.” -
With policymakers:
“Expand access to MAT, decriminalize help-seeking, and regulate over-the-counter sales responsibly.”
💡 The Indian Context
In India, especially:
-
Tapentadol and tramadol are often misused without awareness of risk
-
Pharmacists may act as de facto prescribers
-
Families hide addiction, fearing shame and social exclusion
-
People with mental illness who develop addiction are doubly stigmatized
We need culturally-sensitive, accessible, and non-judgmental services.
💬 Takeaway
Stigma kills more silently than overdose.
To reduce opioid harm in India, we need to stop whispering and start speaking openly—at homes, clinics, classrooms, and communities.
In the final part of this series, we’ll share real recovery journeys, community support options, and how each of us can help someone come back to life.
👨⚕️ About the Author
Dr. Srinivas Rajkumar T, MBBS, MD (Psychiatry)
Consultant Psychiatrist | Apollo Clinics Velachery & Tambaram
Advocate for mental health literacy, deaddiction, and compassionate care
📞 Appointments: 85951 55808
🌐 Resources: www.srinivasaiims.com
📩 Connect: LinkedIn – Dr. Srinivas Rajkumar T