IBS and Mental Health: Understanding the Gut–Mind Axis and Modern Psychiatric Treatment
 Irritable Bowel Syndrome (IBS) is not just a “tummy problem.” It’s a chronic, relapsing condition where psychological health plays a central role. Over the years, research has evolved our understanding of IBS from being a purely gastrointestinal disorder to one that’s deeply rooted in the gut–brain connection.
Irritable Bowel Syndrome (IBS) is not just a “tummy problem.” It’s a chronic, relapsing condition where psychological health plays a central role. Over the years, research has evolved our understanding of IBS from being a purely gastrointestinal disorder to one that’s deeply rooted in the gut–brain connection.
As a psychiatrist, I often work with patients who suffer from long-standing digestive distress that coexists with anxiety, depression, or trauma. Addressing only the gut—or only the mind—is no longer enough. It’s time we embrace a comprehensive, integrated approach.
🌱 IBS Subtypes: Identifying the Pattern Is Key
IBS is classified by bowel habit patterns:
-
IBS-D (Diarrhea-predominant): Frequent loose stools, urgency, and cramps.
-
IBS-C (Constipation-predominant): Hard, infrequent stools with bloating.
-
IBS-M (Mixed-type): Alternating between diarrhea and constipation.
-
IBS-U (Unsubtyped): Doesn’t fit clearly into any subtype.
In addition to these, we also see:
-
Post-Infectious IBS: Develops after acute gastroenteritis.
-
Post-Diverticulitis Functional Changes: Even after the resolution of structural inflammation, altered gut-brain signaling can cause symptoms.
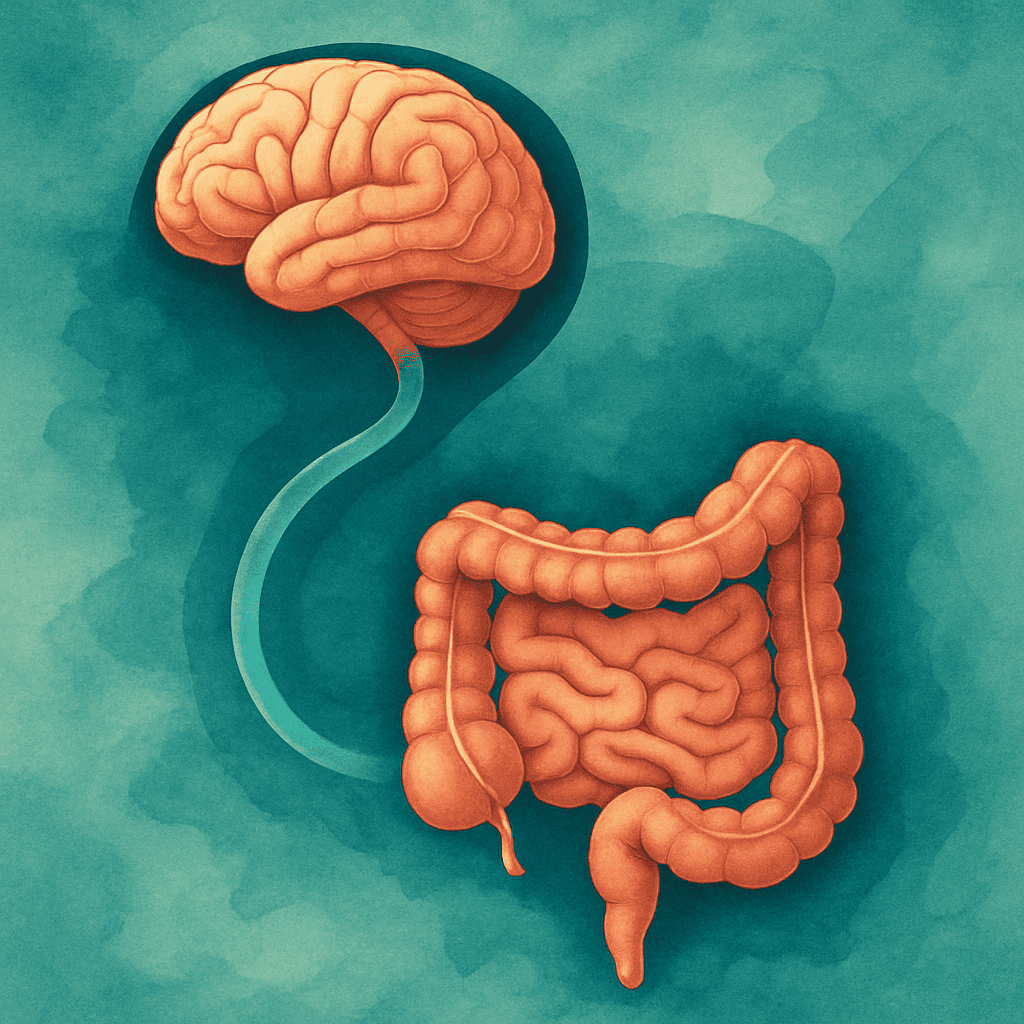
🧠 The Gut–Brain Axis: Two Systems, One Dialogue
Your gut is often called the “second brain.” It’s lined with over 100 million neurons and communicates constantly with the brain through the vagus nerve, hormonal signals, and immune pathways.
🔹 Stress → can slow or speed up gut motility.
🔹 Gut inflammation → can increase anxiety and mood instability.
🔹 Trauma → can sensitize the enteric nervous system.
Up to 90% of IBS patients report psychological symptoms—most commonly:
-
Anxiety disorders
-
Depressive symptoms
-
Somatization and health anxiety
-
Post-traumatic stress, especially in women
🧭 Modern Psychiatric Approach: Science + Sensitivity
Treating IBS requires a psychiatric approach that’s biopsychosocial—addressing biological, psychological, and social aspects. Let’s break it down.
1. Screening for Underlying Psychological Conditions
It’s important to screen for:
-
Generalized Anxiety Disorder (GAD)
-
Major Depressive Disorder (MDD)
-
Panic disorder
-
Somatic Symptom Disorder
-
Health anxiety or hypochondriasis
Validated tools such as PHQ-9, GAD-7, and the IBS Severity Scoring System (IBS-SSS) help guide treatment plans.
💊 Psychiatry Medications in IBS: A Functional, Not Just Mood-Based Approach
Psychotropic medications in IBS are not used only for psychiatric symptoms. Many of them have neuromodulatory effects on the gut.
👉 Tricyclic Antidepressants (TCAs)
Examples: Amitriptyline, Nortriptyline, Imipramine
-
Dose: Low (e.g., 10–50 mg at bedtime)
-
Mechanism: Anticholinergic effect slows gut motility—helpful in IBS-D.
-
Other benefits: Pain modulation, sleep improvement.
Caution: May worsen constipation in IBS-C, and cause dry mouth or drowsiness.
👉 Selective Serotonin Reuptake Inhibitors (SSRIs)
Examples: Sertraline, Escitalopram, Fluoxetine
-
Dose: Standard antidepressant range
-
Mechanism: Improves overall mood and pain tolerance; helpful in IBS-C due to prokinetic effect.
-
Advantages: Better tolerated than TCAs, especially in younger or anxious individuals.
👉 SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors)
Examples: Duloxetine, Venlafaxine
-
Used for: Coexisting chronic pain syndromes (e.g., fibromyalgia, pelvic pain), anxiety with IBS.
-
Note: Has antidepressant and central pain-relieving effects.
👉 Anxiolytics (Short-Term Use Only)
Examples: Clonazepam, Etizolam (only short courses)
-
Used very sparingly for acute anxiety spikes. Not for long-term use due to dependence risk.
👉 Atypical Antipsychotics (Low Dose Off-Label)
Examples: Olanzapine (low dose), Quetiapine
-
Used rarely in IBS patients with significant health anxiety, sleep issues, or somatic preoccupations that don’t respond to standard treatments.
👉 Probiotic Psychobiotics (Emerging Area)
Some probiotics (like Bifidobacterium longum and Lactobacillus rhamnosus) may influence the brain via the gut and reduce anxiety—a field called psychobiotics.
💬 Psychological Therapies: Healing the Emotional Underbelly
Even the best medications won’t work well if emotional triggers are not addressed.
🧠 Cognitive Behavioral Therapy (CBT)
-
Targets catastrophizing about symptoms, fear-avoidance behaviors, and improves emotional regulation.
-
Often delivered in 8–12 sessions. Virtual options also work.
🌿 Mindfulness-Based Stress Reduction (MBSR)
-
Helps reduce visceral hypersensitivity and autonomic arousal.
-
Includes breath work, body scans, and guided relaxation.
🤝 Trauma-Focused Therapy
-
Especially helpful in women with IBS and a history of abuse, neglect, or medical trauma.
🧩 Integrated Care: The Way Forward
Multidisciplinary teams deliver better outcomes. The ideal IBS care team may include:
-
Gastroenterologist
-
Psychiatrist
-
Clinical Psychologist
-
Dietician (especially for low FODMAP guidance)
When patients feel seen, heard, and believed, outcomes improve.
❤️ Final Word: Treating IBS Is Treating the Whole Person
IBS is a deeply personal condition. Each patient’s symptom flare has a story—stress, food triggers, lifestyle disruptions, or past trauma. Treating it with empathy and science—by integrating gut and mental health—is the only path to lasting relief.
If you or someone you love struggles with IBS, know that help is available. And it doesn’t begin only in the gut—it starts in the mind too.
Dr. Srinivas Rajkumar T
MD (AIIMS, New Delhi), Consultant Psychiatrist
📍 Apollo Clinic, Opp. Phoenix Marketcity, Velachery, Chennai
☎️ +91 8595155808
🌐 www.srinivasaiims.com