Schizotypy Explained: Traits, Models, and Measurement Tools
 When people hear the word schizophrenia, they often imagine a sharp line between “ill” and “healthy.” Modern psychology tells a more interesting story. That story begins with schizotypy.
When people hear the word schizophrenia, they often imagine a sharp line between “ill” and “healthy.” Modern psychology tells a more interesting story. That story begins with schizotypy.
What Is Schizotypy?
Schizotypy refers to a set of inherited personality traits that resemble, in milder form, the symptoms seen in schizophrenia. These traits do not automatically mean illness. Instead, schizotypy represents a continuum of vulnerability—what researchers call an endophenotype—that may or may not progress to clinical psychosis.
Think of schizotypy as the soil. Illness may grow from it, but only under certain conditions.
Three Major Models of Schizotypy
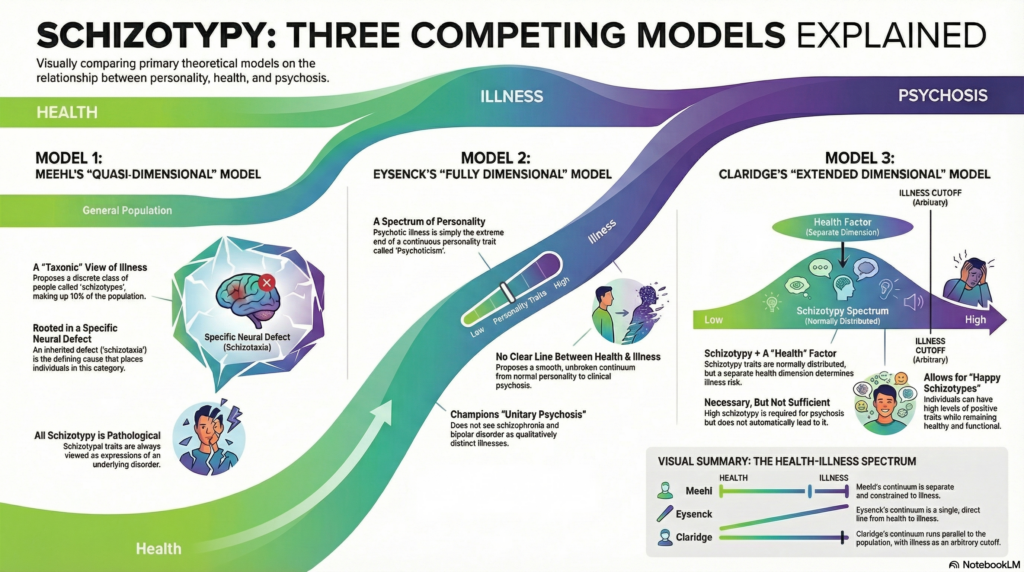
Over time, researchers have proposed different ways of understanding how schizotypal traits relate to mental health and illness.
1. The Meehlian Model (Quasi-Dimensional / Taxonic)
Proposed by Paul Meehl, this model suggests that a distinct subgroup of people, called schizotypes, carry a specific genetic vulnerability.
According to this view:
-
A genetic factor (often called the schizogene) leads to a neural condition termed schizotaxia.
-
Around 10% of the population may carry this vulnerability.
-
Only about 1% will go on to develop schizophrenia.
Health and illness are relatively distinct here. Schizotypy is seen as a graded form of underlying disorder, not merely normal variation.
2. The Eysenckian Model (Fully Dimensional)
Hans Eysenck took a very different stance.
In this model:
-
Psychosis lies at the extreme end of normal personality traits.
-
Everyone falls somewhere along dimensions such as Psychoticism, Extraversion, and Neuroticism.
-
There is no separate “schizotypy” construct—only extreme personality configurations.
Illness is not categorically different from health; it is simply too much of the same thing.
3. Claridge’s Model (Dimensional with a Health Filter)
Gordon Claridge refined the dimensional view further.
Claridge proposed that:
-
Schizotypal traits are normally distributed across the population.
-
High schizotypy alone does not cause illness.
-
A second factor—psychological and biological resilience (“health”)—determines whether traits become pathological.
This model introduced the idea of “happy schizotypes”: individuals with unusual perceptions or beliefs who experience them as enriching rather than distressing.
The Three Core Dimensions of Schizotypy
Across models, schizotypy is commonly divided into three trait clusters:
-
Positive schizotypy: unusual experiences, perceptual distortions, magical thinking
-
Negative schizotypy: social withdrawal, emotional flatness, lack of pleasure
-
Disorganized schizotypy: odd speech, cognitive slippage, eccentric behavior
Different combinations of these traits can lead to very different outcomes.
How Is Schizotypy Measured?
Researchers choose assessment tools based on their theoretical framework:
-
Wisconsin Schizotypy Scales (WSS)
Rooted in the Meehlian model, focusing on traits closely tied to psychopathology. -
Schizotypal Personality Questionnaire (SPQ)
Based on DSM criteria for schizotypal personality disorder. -
Oxford–Liverpool Inventory of Feelings and Experiences (O-LIFE)
Based on Claridge’s model, treating schizotypy as normal personality variation, including a distinct disorganization scale.
A Helpful Analogy: Blood Pressure
Claridge offered a powerful metaphor. Everyone has blood pressure, and it varies naturally. Only when it crosses a critical threshold does it become hypertension.
Schizotypy works the same way. Traits are widespread and often benign. Illness emerges only when multiple vulnerabilities cluster together and overwhelm the system.
Why This Matters
Understanding schizotypy helps clinicians and researchers move beyond black-and-white thinking. It reminds us that:
-
Vulnerability is not destiny
-
Traits can be adaptive or impairing depending on context
-
Early identification can focus on resilience, not just risk
About the Author
Dr. Srinivas Rajkumar T
MD (AIIMS), DNB, MBA
Consultant Psychiatrist & Neurofeedback Specialist
Mind & Memory Clinic, Apollo Clinic Velachery (Opp. Phoenix Mall)
I work at the intersection of clinical psychiatry, neuroscience, and dimensional models of mental health—focusing on early identification, functional assessment, and personalized interventions rather than labels alone.
📞 +91-8595155808
✉ srinivasaiims@gmail.com